Insurance Coverage For Rapid Covid Test
According to its website UnitedHealthcare members will have 0 cost-share copay coinsurance or deductible for COVID-19 testing-related visits through Jan. Tests to diagnose or aid the diagnosis of COVID-19.

Your Covid Testing Faq Answered Excel Urgent Care
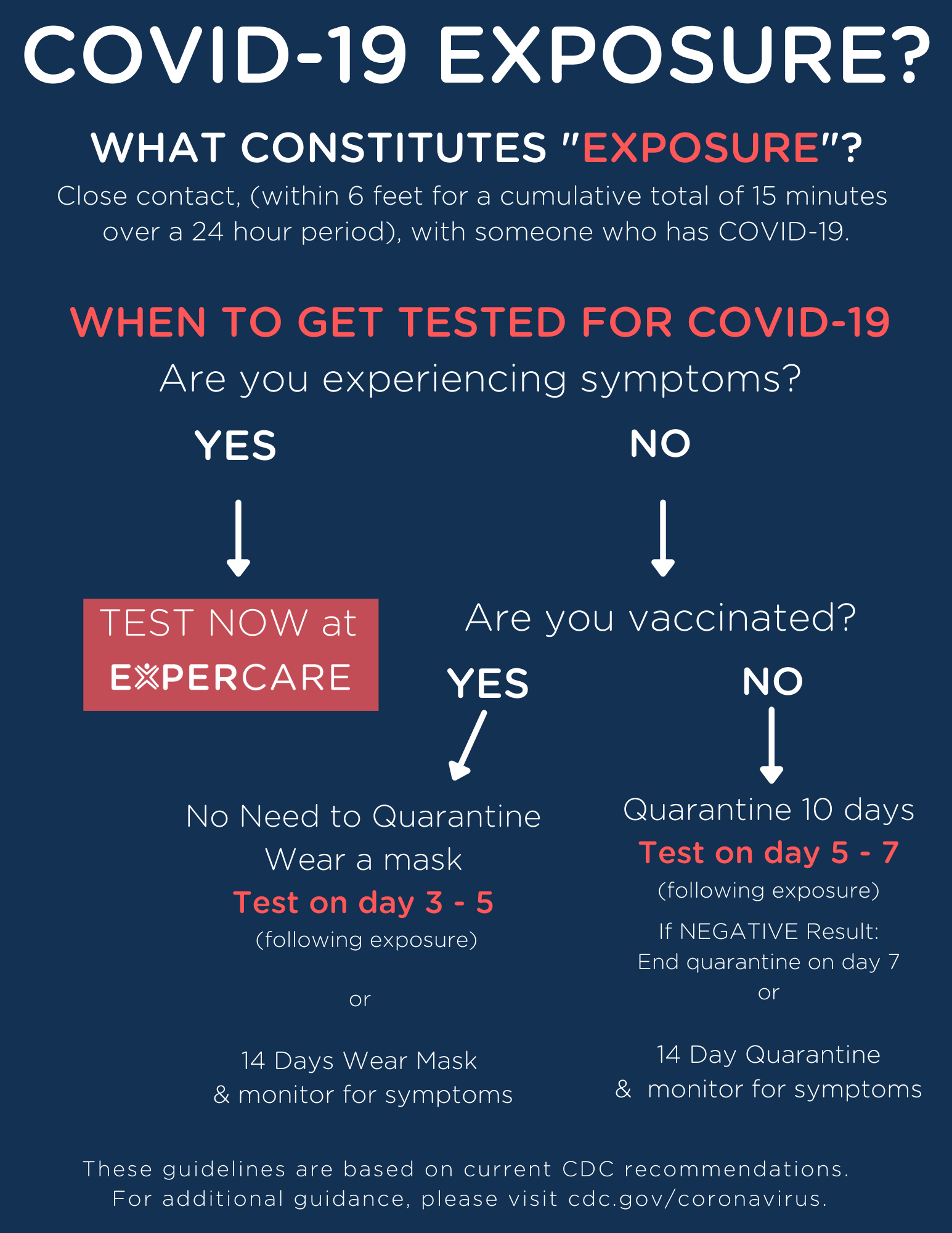
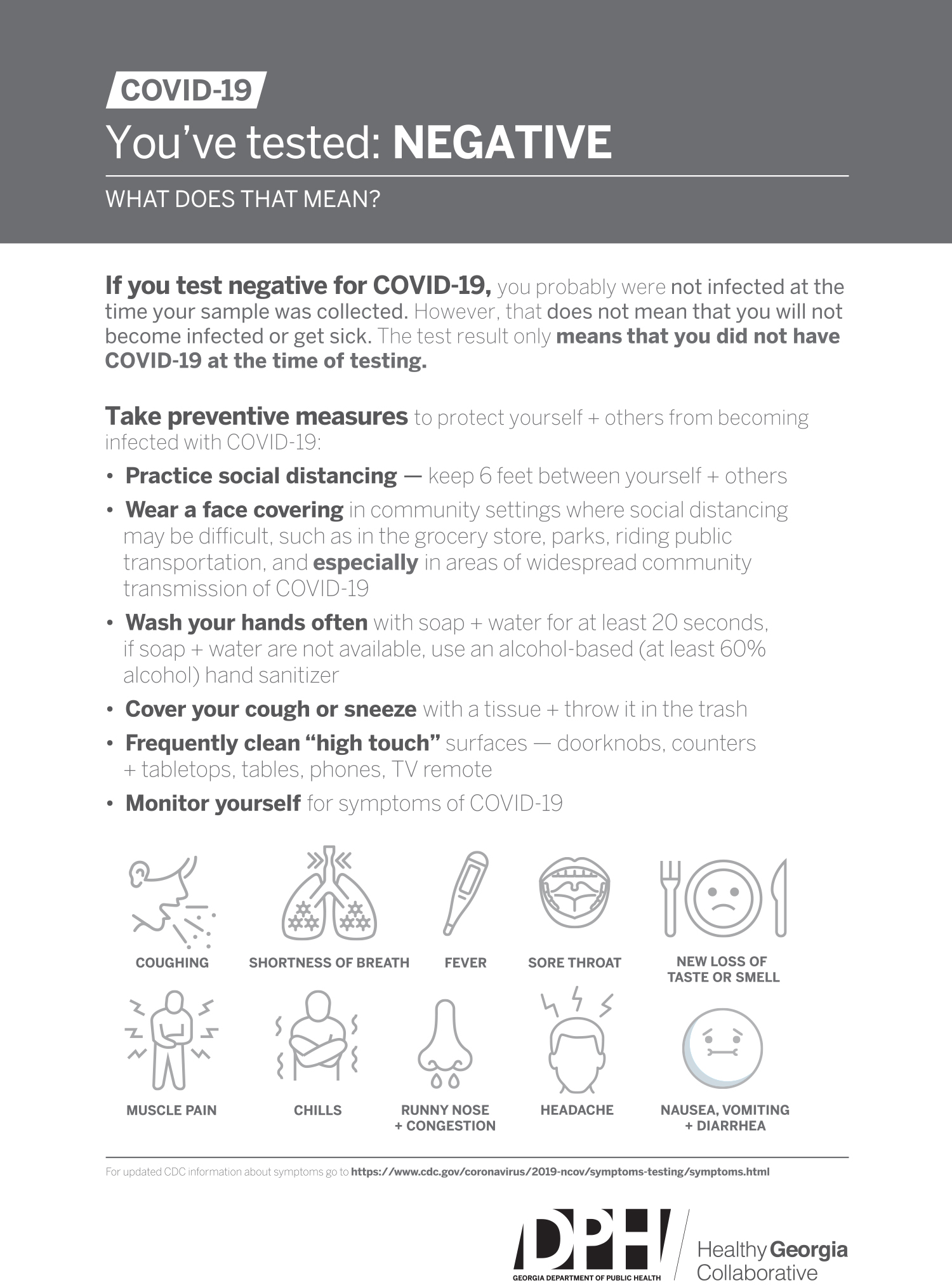
An antibody test may determine if a person has been exposed to COVID-19 while a COVID-19 diagnostic test determines if a person is currently infected.

Insurance coverage for rapid covid test. Loren Adler and Christen Linke Young examine the existing coverage for COVID-19 testing outline ways to improve access and propose how to better finance COVID-19 testing in the future. Rapid point of care antigen tests where results are available within a few minutes Home test kits when ordered by a. FDA authorized tests include tests approved for patient use through pre-market approval or emergency use pathways and tests that are developed and administered in accordance with FDA specifications or through state regulatory approval.
When tests are available for you in your state Medicare covers and you pay nothing for. COVID-19 vaccines are 100 free for every individual living in the United States - even if you do not have insurance. You do not need to obtain a referral from a physician in order to get a COVID-19 test and have it covered by Medicare.
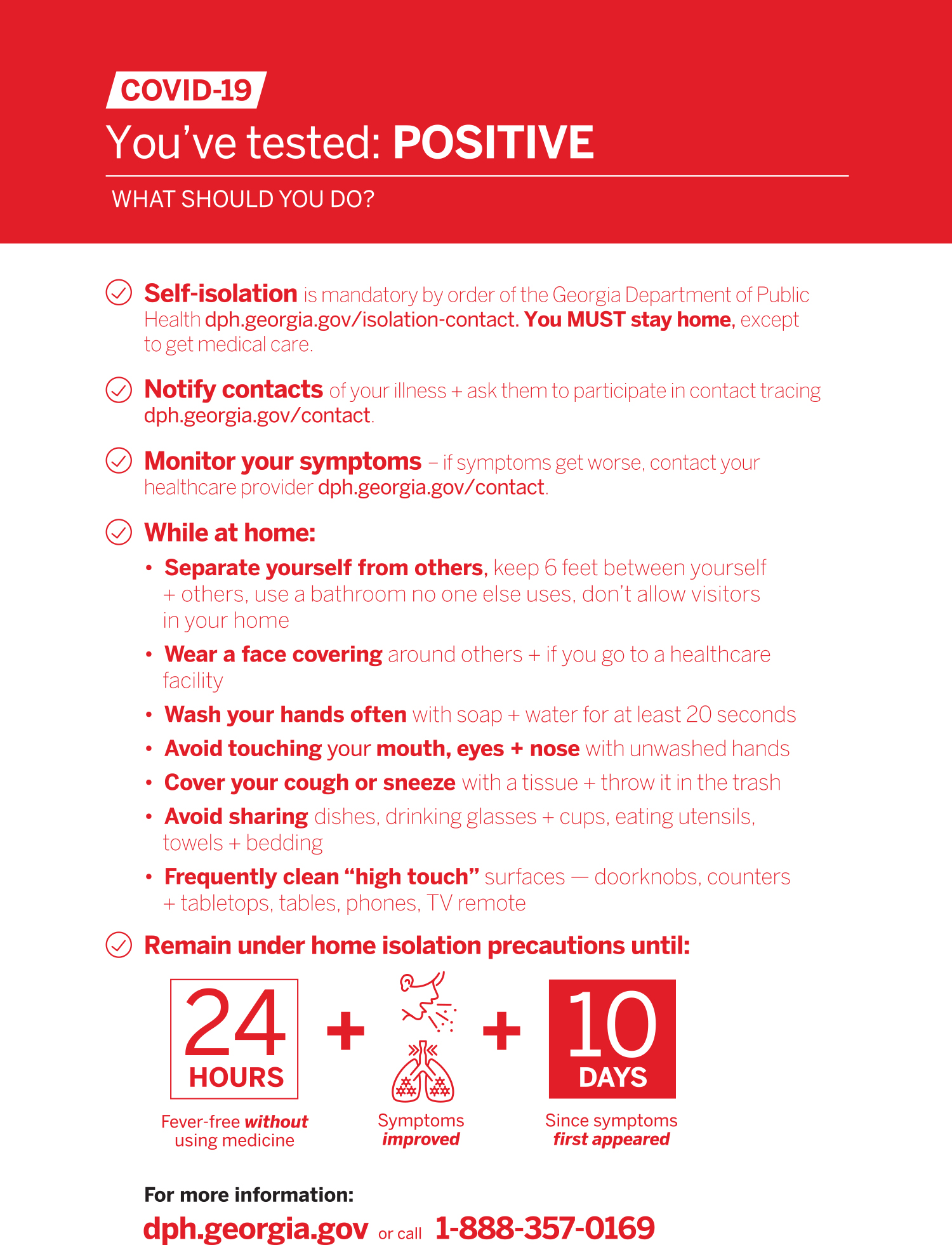
A test must be covered if your attending health care provider has assessed your individual situation and determined that it is medically appropriate you have symptoms or have a known or likely recent exposure to COVID-19. Original Medicare covers COVID-19 testing with no out-of-pocket Medicare costs to you. If your doctor or other health care professional provides a prescription or order for the over-the-counter COVID-19 test as part of clinical care you may submit a claim for reimbursement with both the prescription and detailed receipt to UnitedHealthcare.
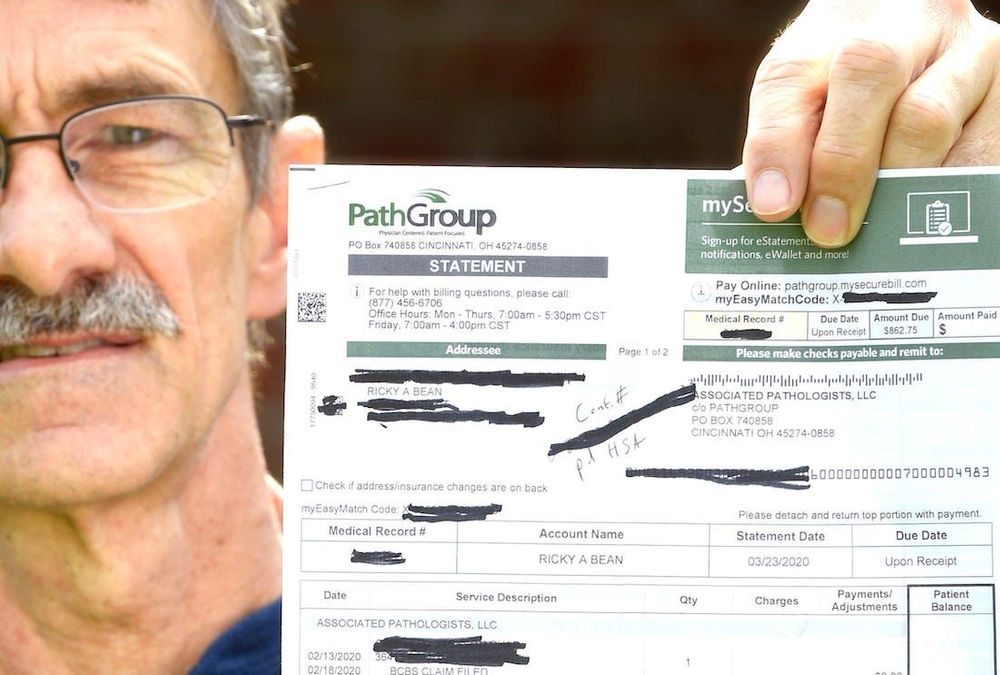
Doctors typically charge about 50 to 100 for the tests so the costs of weekly testing could add up quickly. Many insurers have also agreed to cover the cost of a COVID test if its done at an out-of-network facility but youll want to reach out to your insurance company or MedicareMedicaid provider before your visit. Americas Health Insurance Plans is calling on more government support to cover the cost of COVID-19 tests which it says could be between 6 billion and.
Cigna covers medical care for COVID-19 treatment subject to standard cost share copay and deductibles. Your primary care provider may be willing to test you for COVID-19 if you dont have symptoms although your insurance may not cover the test or the cost of the office visit for this purpose. Youll need a negative COVID-19 viral test to re-enter the United States as well.
Health insurance issuers and group health plans must cover COVID- 19 diagnostic testing as determined medically appropriate by the individuals health. Which types of COVID-19 diagnostics tests are covered. 2 Rapid-result tests can be pricey costing up to 250 and often arent covered by health insurance.
State variations and regulations may apply. Insurers are legally required to pay for in-network testing so try to find a medical facility where you know youll be covered. Blue Shield and Blue Shield Promise cover these diagnostic tests.
Medicaid Keystone First Health Partners Aetna Better Health UHC Community Plan Generally Rapid COVID-19 testing is not covered but standard NAA testing is usually covered. Medicare covers these tests at different locations including some parking lot test sites. If you do not have health insurance talk to any health care provider in your area to see if they will agree to bill the federal government for other COVID-19.
Laboratories that complete a majority of COVID-19 diagnostic tests run on high throughput technology within two days will be paid 100 per test by Medicare while laboratories that take longer will receive 75 per test. C ontact your insurance company. And second youre in luck.
Some tests for related respiratory conditions to aid diagnosis of COVID-19 done together with the COVID-19 test. Only those COVID-19 vaccine administration claims denied or not fully paid by a patients health insurance plan including those insurance plans with patient co-pays for vaccine administration deductibles for vaccine administration or co-insurance related to COVID-19 vaccination are eligible for reimbursement by the HRSA COVID-19 Coverage Assistance Fund. Federal law requires insurers to fully cover the tests when ordered by a.
Cigna covers out-of-pocket expenses for a covered COVID-19 diagnostic visit and testing with no customer cost share through the Public Health Emergency PHE period currently scheduled to end on October 18 2021. Medicaid patients may not pay out of pocket for Rapid COVID Testing. Standard PCR tests sent to a lab.
Patients who are exhibiting symptoms of COVID-19 or have been exposed to someone who has recently tested positive for the virus can visit AFC Urgent Care Conshohocken for COVID-19 rapid diagnostic testing. And over at Allianz Global Assistance which offers COVID-19 insurance and assistance for clients who test positive for COVID-19 while travelling a COVID-19 test will only be. Under the terms of the Families First Coronavirus Response Act HR6201 Medicare Medicaid and private health insurance plans including grandfathered plans are required to fully cover the cost of COVID-19 testing without any cost-sharing or prior-authorization requirements for the duration of the emergency period which has most recently been extended through mid-April 2021.
While no single authority would confirm that every insurance company will reimburse 100 for rapid COVID tests we confirmed large healthcare insurers Aetna Cigna and. If you have health care coverage directly from an insurance company the health insurance marketplace or through your employer including through COBRA. Tests for the coronavirus are covered by Medicare Part B much like many other tests and screenings.
Congress required health plans to fully cover COVID-19 testing but insurance companies are starting to argue they should only have to pay if patients show symptoms or tests are ordered by a. Our center performs rapid testing using the Abbott ID NOW diagnostic test which allows us to provide patients with results. Many airports are now offering test sites.
Some that charge travelers for rapid and PCR tests and some that offer complimentary screenings for travelers.
How Much Does A Rapid Covid 19 Test Cost Without Insurance Mira

Rapid And Affordable Covid 19 Tests 75 Antigen And Antibody Tests Results In 30 Minutes Or Less Accel Diagnostics

How Americans Can Get A Covid Test In Mexico The Washington Post
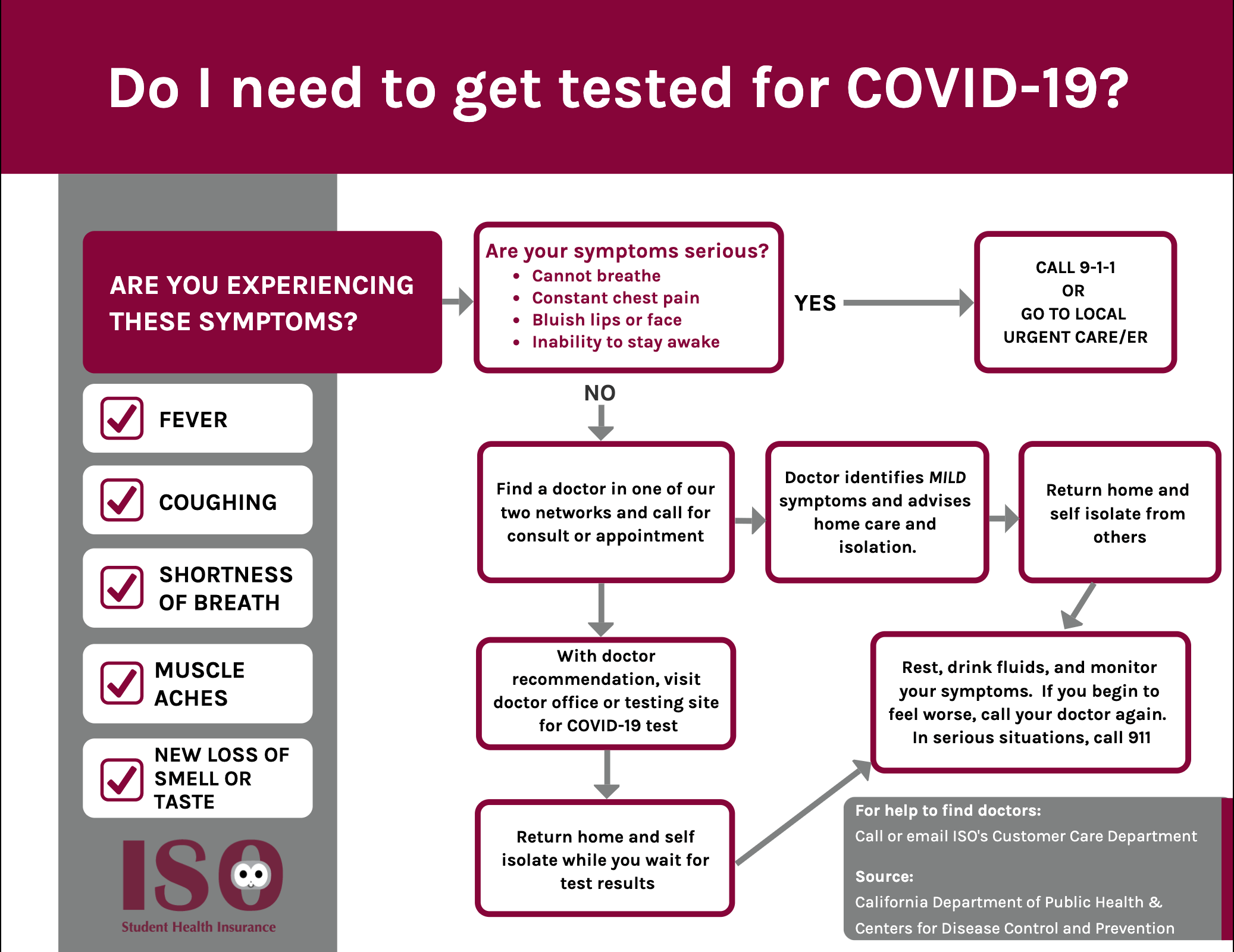
Iso International Student Insurance

Coronavirus Faq For Wellfleet Student Members Wellfleet Student
.jpg)
Covid 19 Pcr And Antigen Tests Los Cabos

Covid 19 Pcr And Antigen Tests Los Cabos
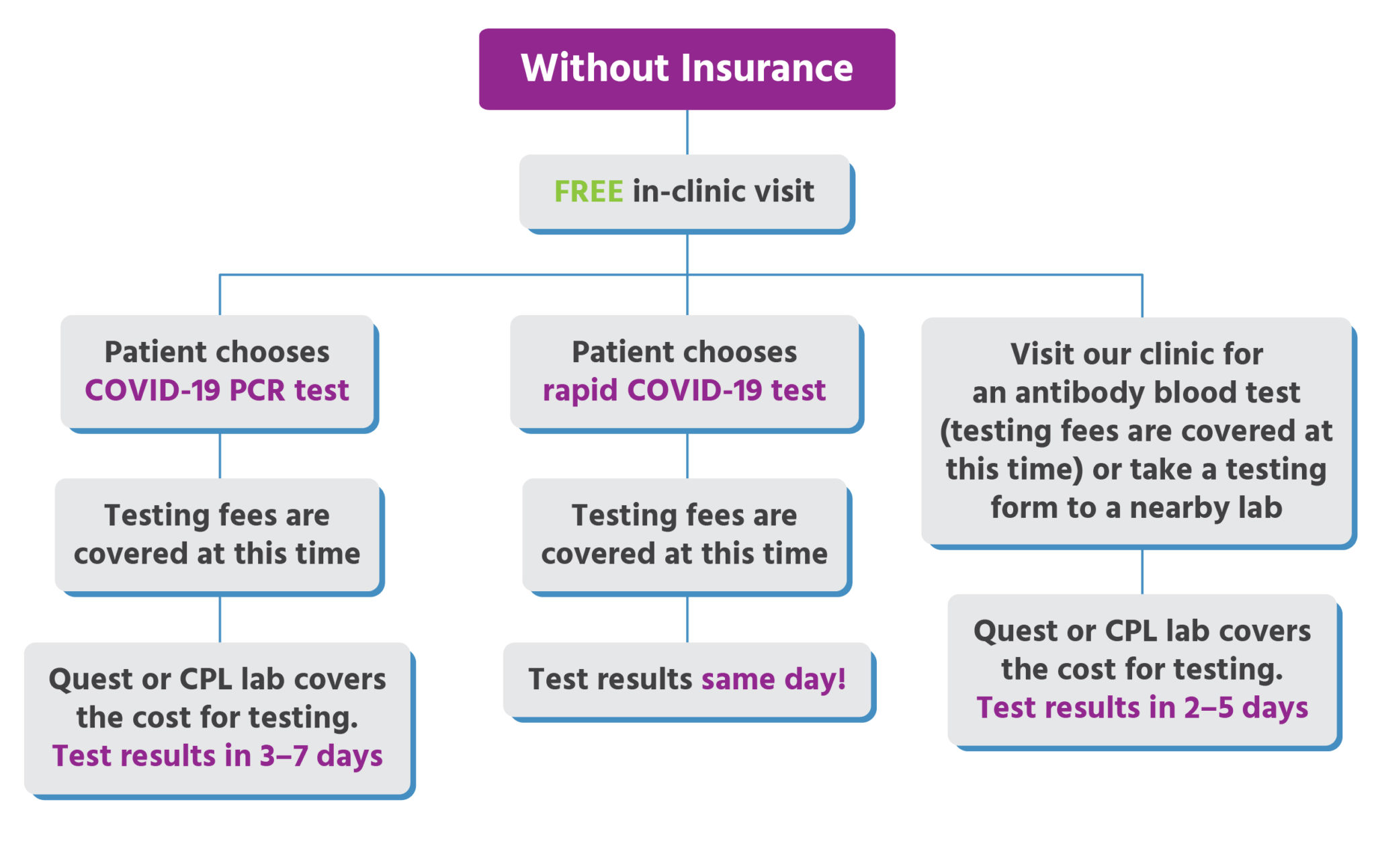
Urgent Care For Kids Free Care For Uninsured Families

Covid Testing Where To Get Tested In San Francisco Bay Area
Covid 19 Services Promptmd Hoboken Edgewater Jersey City Nj

Five Things To Know About The Cost Of Covid 19 Testing And Treatment Kff

Covid 19 Testing And Covid Antibody Testing Stat Med Urgent Care

Testing For Covid 19 Faqs Blue Shield Of Ca

Pharmacy Hours Online Services Coronavirus Updates City Market
Faqs On Medicare Coverage And Costs Related To Covid 19 Testing And Treatment Kff

Chicago Covid Testing Rapid Covid 19 Tests Drive Up Screening Clinic
Posting Komentar untuk "Insurance Coverage For Rapid Covid Test"