Insurance Coverage Step Therapy
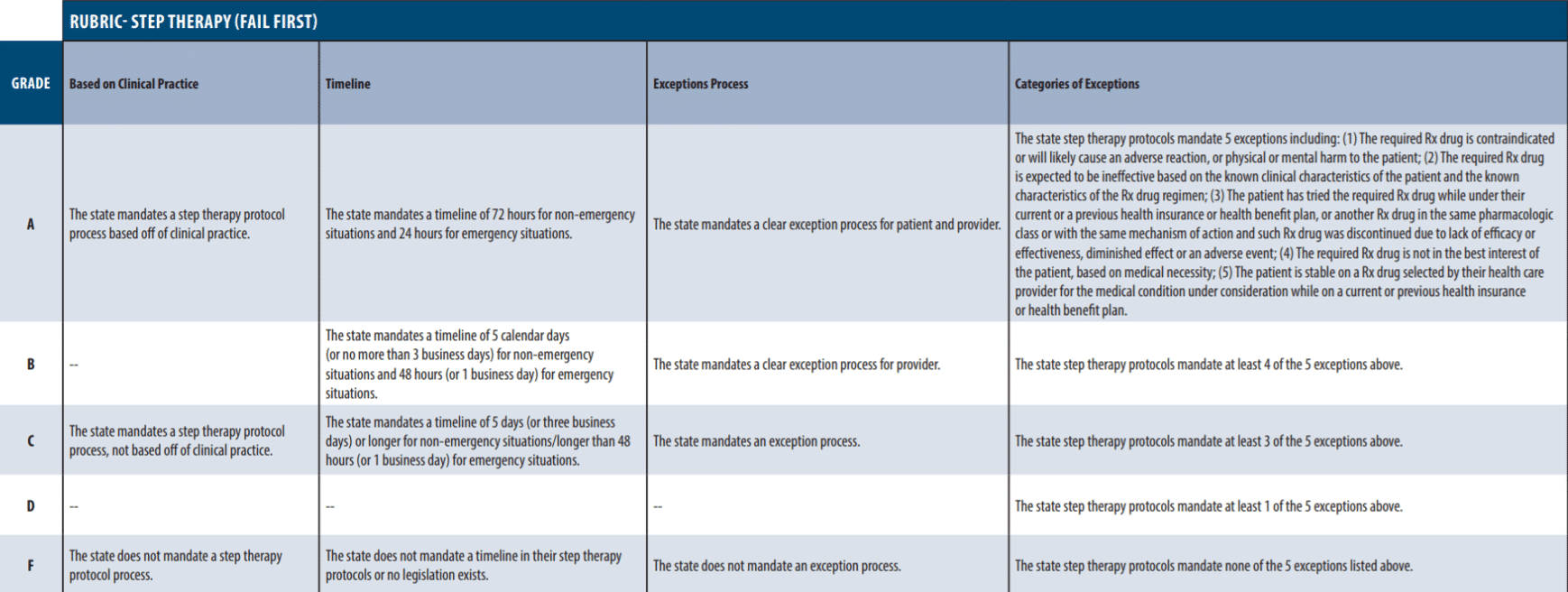
Step therapy also known as fail first is a form of prior authorization. For these reasons private health insurance companies that offer prescription drug coverage sometimes set quantity limits.

Insurance Coverage And Financing Landscape For Hiv Treatment And Prevention In The Usa The Lancet
Step therapy programs are utilized to encourage use of lower cost alternatives for certain therapeutic classes.
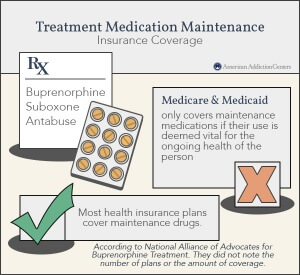
Insurance coverage step therapy. Each Medicare Part D plan has a list of covered drugs that are called a formulary. 72016 Added Indiana and West Virginia coverage information. What does step therapy mean in Medicare drug coverage.
If your state has not mandated override processes or. In most cases you must first try a less expensive drug on the Medicare Prescription Drug Plans formulary also called a drug list that has been proven effective for most people with your condition before you can move up a step to a more expensive drug. Added California coverage information.
If that doesnt help you try a Tier 1 medicine. Step therapy requires prior authorization for drugs that are prescribed for some medical conditions. If you have health insurance through your job it may or may not include coverage for therapy.
Under the health insurance policy. Prohibiting step therapy. 5 2017 Annual Review.
Some patients suffer terribly during this process becoming. Lets say youre having allergy problems. 4 Step therapy exception means the exception to the step therapy process and the determination of whether the exception will be granted taking into consideration the insureds needs and medical circumstances along with the professional judgment of the insureds provider.
Requirement for coverage of step therapy or fail first protocols. Patients start with older cheaper treatments and if they are not effective patients step to another treatment. Program Step Therapy - Vraylar cariprazine Change Control 42016 New program.
221047 to the contrary any health care coverage plan specified in Subsection D of this Section which includes prescription benefits as part of its policy or contract which utilizes step therapy or fail first protocols and which is issued for delivery delivered renewed. Changed brand Seroquel XR to generic formulation and updated references. A few states prohibit step therapy entirely depending on the diagnosis of the patient.
Notwithstanding the provisions of RS. Step therapy means trying less expensive options before stepping up to drugs that cost more. Step therapy may sound like an exercise program but it actually refers to managed care for prescription drug therapies and a process that healthcare insurers use to control prescription drugs costs.
Step therapy prevents patients from accessing treatments prescribed by their doctor and instead mandates a course of treatment mandated by their insurance carrier. Even if you have coverage its up to you to decide whether or not you wish to use it. Colorado prohibits all insurance companies from using step therapy.
Step therapy is a type of prior authorization. Please see table below use the Janssen CarePath Provider Portal or contact Janssen CarePath at 877-CarePath 877-227-3728 for assistance in obtaining PA forms. The Committee on Insurance and Real Estate reported through SEN.
Step therapy is also known as step protocol or a fail first requirement. Taking too much medicine or taking it too often may worsen your health condition and increase your health care costs. An independent company that provides a secure web-based portal between providers and health insurance companies.
Your doctor must prescribe a less expensive step-one drug such as over-the-counter or generic medications first. Doctors say insurance companies are undermining patient health When he was diagnosed with two autoimmune diseases Joel Hechler knew hed be in for a battle. If you are denied coverage you.
Ingrezza and Austedo are both a vesicular monoamine transporter 2 VMAT2 inhibitor s. North Dakota and Utah prohibit step therapy for patients diagnosed with metastatic cancer. Heres what step therapy looks like.
An online marketplace for health insurance plans. You should first try using an over-the-counter medication. Additional information on the PA process at major payers is shown below.
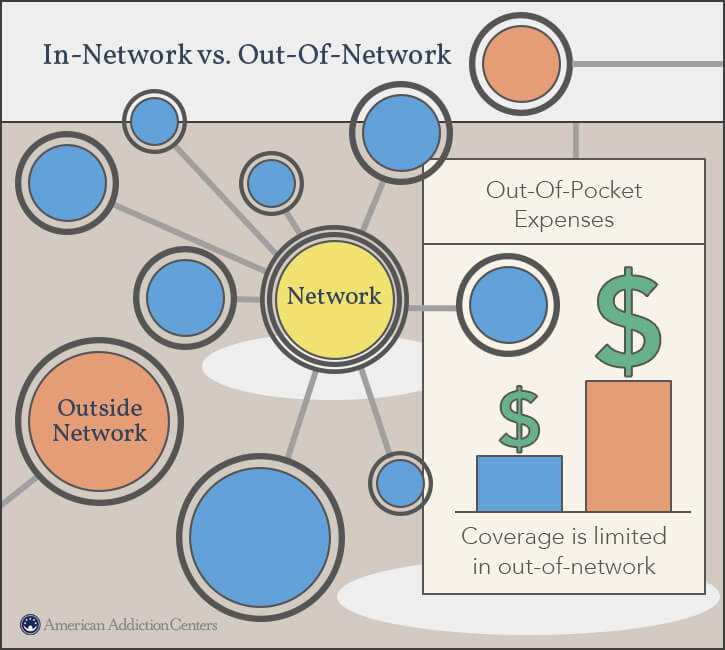
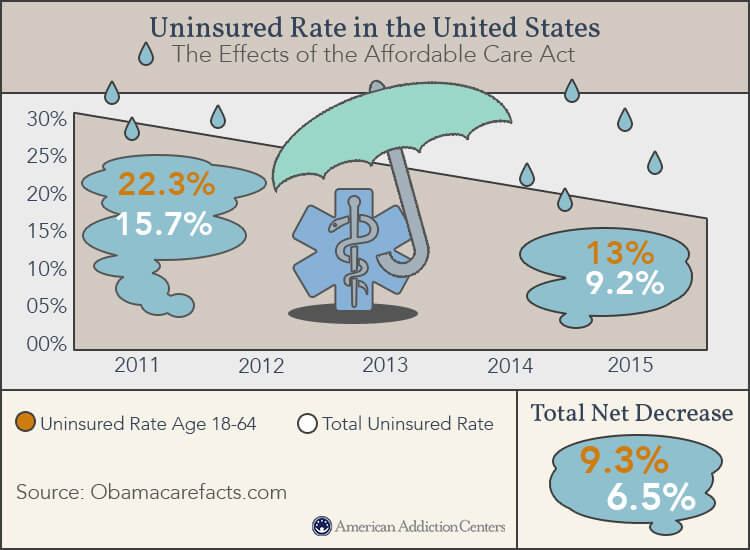
A decision to override a generally applicable step therapy protocol in favor of coverage of the. To reduce the use of expensive medications insurers have long relied on step therapy a restriction on insurance coverage that requires patients to prove that less-expensive drugs are ineffective before getting coverage for a more expensive higher-tier drug. If it doesnt work ie it fails then your insurance will consider covering a costlier drug like a lower-cost brand-name medicine.
Heres an example of step therapy. Benefit plan issuer that requires a step therapy protocol before providing coverage for a prescription drug must establish implement and administer the step therapy protocol in accordance with clinical review. The information provided is not a guarantee of coverage or payment partial or full.
LESSER of the 9th Dist Chairperson of the Committee on the part of the Senate that the bill ought to pass. MEDICARE ADVANTAGE PROVIDERS STEP THERAPY PRIOR AUTHORIZATION REQUIREMENTS FOR MEDICARE ADVANTAGE Beginning April 1 2019 step therapy prior authorization requirements will be added to the select drugs on the list below. It is implemented by prescription drug insurance providers by using the.
AN ACT CONCERNING STEP THERAPY ADVERSE DETERMINATION AND UTILIZATION REVIEWS AND HEALTH INSURANCE COVERAGE FOR CHILDREN STEPCHILDREN AND OTHER DEPENDENT. This program requires a member to try Austedo before providing coverage for Ingrezza for the treatment of tardive dyskinesia. Within every formulary there are a set of rules applied to the prescription drugs covered by the plan.
MA plans participating in Part B step therapy must disclose that Part B drugs may be subject to step therapy requirements in the plans Annual Notice of Change ANOC and Evidence of Coverage EOC documents that are provided to enrollees prior to the Medicare Open Enrollment period to assist them in making plan selections for the upcoming year.

Does Health Insurance Cover Occupational Therapy Quotewizard

Medicare Part B Drug Requirements Coverage Step Therapy

The Addiction Continuum Of Care Foundations Recovery Network
What Is Step Therapy How To Get Insurance To Pay For Your Non Preferred Drug Goodrx
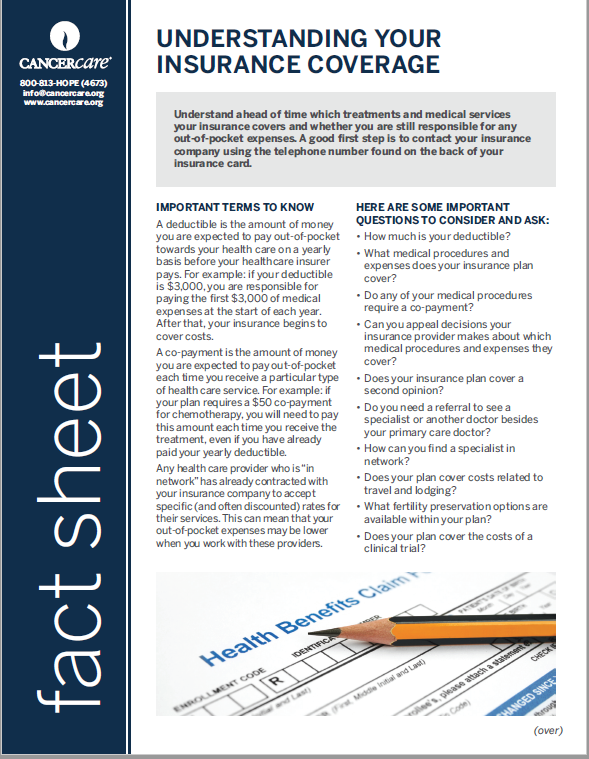
Understanding Your Insurance Coverage
What Is Step Therapy How To Get Insurance To Pay For Your Non Preferred Drug Goodrx

Fail First Step Therapy 50 State Network

Fail First Step Therapy 50 State Network
Rehab Insurance Does Insurance Cover Drug Alcohol Rehab
Step Therapy Fail First Nord National Organization For Rare Disorders

Steps Of The Health Technology Assessment Hta Research Process And Download Scientific Diagram
Rehab Insurance Does Insurance Cover Drug Alcohol Rehab
![]()
Step Therapy Fail First Nord National Organization For Rare Disorders
Rehab Insurance Does Insurance Cover Drug Alcohol Rehab
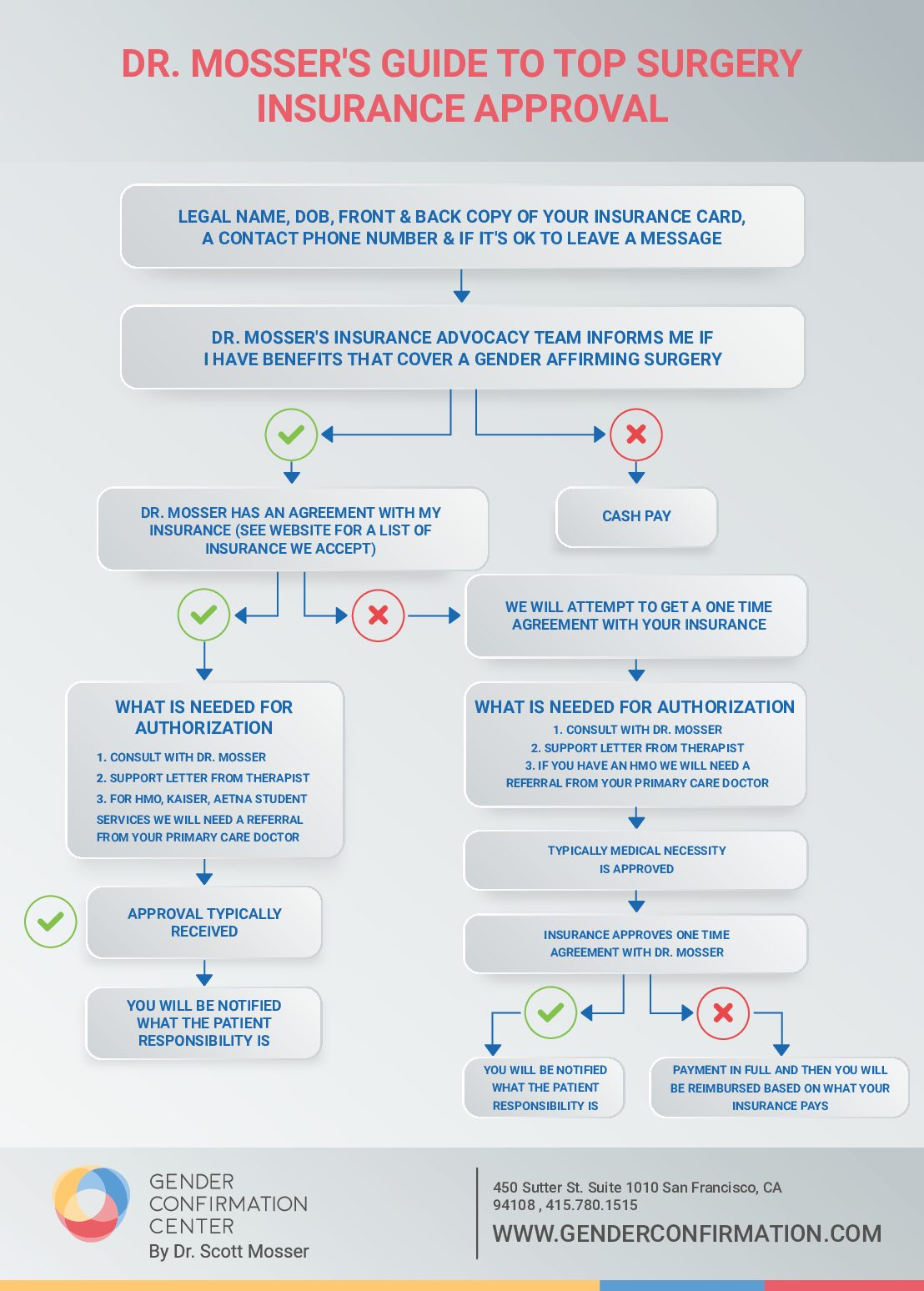
Insurance Approval Gender Confirmation
How Do Insurance Companies Reimburse For Therapy Master Class Ch 2
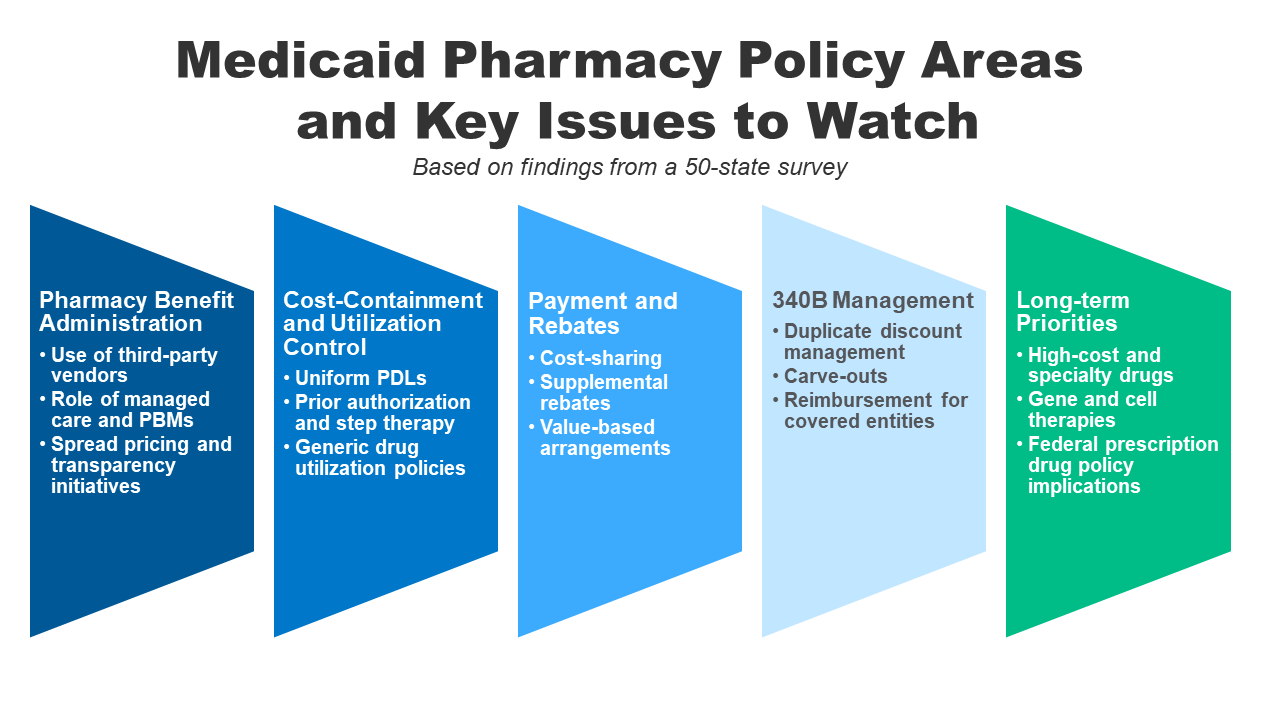
How State Medicaid Programs Are Managing Prescription Drug Costs Cost Containment And Utilization Control Strategies 9439 Kff

Step Therapy National Infusion Center Association

Posting Komentar untuk "Insurance Coverage Step Therapy"