Does My Insurance Cover Covid Testing Ambetter
Yes when medically necessary diagnostic testing is ordered andor referred by a licensed health care provider your Ambetter plan will cover the cost of COVID-19 tests and the associated physicians visit. When medically necessary diagnostic testing or medical screening services are ordered andor referred by a licensed health care provider your Ambetter plan will cover the cost of medically necessary COVID-19.

Manuals And Forms Ambetter From Peach State Health Plan
Centene will cover COVID-19 testing and screening services for Medicaid Medicare and Marketplace members and is waiving all associated member cost share amounts for COVID-19 testing and screening.

Does my insurance cover covid testing ambetter. Call the member service information number located on the back of your insurance card. If you end up needing assistance after your insurance has been billed please reach out to them at 855 685-5227 to apply. Those with Original Medicare only will generally not be covered outside the US although additional coverage is available.
Please also know that Molecular Testing Labs has a generous financial aid plan. The good news is that Travel Medical Insurance plans can help cover the cost of medical care. Therefore Blue Cross plans will cover outpatient COVID-19 testing and treatment as well as all telehealth visits without charging members any.
If you have an HPV kit you may be billed 60-80 as an expected allowable. Business interruption coverage requires related property damage. Heres How to Check.
Call us 833 541-5757. Health care providers who have conducted COVID-19 testing for uninsured individuals provided treatment to uninsured individuals with a primary COVID-19 diagnosis on or after February 4 2020 or administered an FDA-authorized or licensed COVID-19 vaccine to uninsured individuals can request claims reimbursement through the program electronically and are reimbursed generally at Medicare. Most health insurance plans require a co-payment at the time of service.
The Affordable Care Act requires health plans that started on or after September 23 2010 to cover colorectal cancer screening tests which includes a range of test options. For now comprehensive insurance carriers will also cover hospitalizations related to the COVID-19 virus and COVID-related telemedicine services which have skyrocketed during the COVID. Does my Ambetter plan cover COVID-related services.
When medically necessary diagnostic testing medical screening services andor treatment is ordered andor referred by a licensed health care provider we will cover the cost of medically necessary COVID-19 tests screenings associated physicians visits andor treatment. In some cases Medicare will cover necessary care if. Does my Ambetter plan cover COVID-related services.
Many insurers have also agreed to cover the cost of a COVID test if its done at an out-of-network facility but youll want to reach out to your insurance company or MedicareMedicaid provider before your visit. Please bring a valid ID and proof-of-insurance if you plan to use health insurance to pay for your visit. We recommend contacting your insurance company before your visit to verify coverage for the specific service youre seeking.
Private health insurance coverage for colorectal cancer screening. CareNow urgent care clinics accept most insurance plans we will file your claim to make the insurance process as easy as possible. The company will not require prior authorization prior certification prior notification or step therapy protocols for these services.
Standard travel insurance will not offer trip cancellation for government mandated travel restrictions either. Be sure to review plan documents before purchasing a plan. Help speed access to COVID-19 testing and treatment and encourage the use of telehealth instead of in person visits to stop the spread of COVID-19.
Does my plan cover COVID-19 testingscreeningtreatment services. Your state department of health website listed below is the best way to know when you are eligible for the vaccine and how to schedule it. This will prepare you for any out-of-pocket costs including co-pays and deductibles that you might be responsible for.
If no testing is performed providers may still bill for COVID-19 screening visits for suspected contact using the following Z codes. Under the terms of the Families First Coronavirus Response Act HR6201 Medicare Medicaid and private health insurance plans including grandfathered plans are required to fully cover the cost of COVID-19 testing without any cost-sharing or prior-authorization requirements for the duration of the emergency period which has most recently been extended through mid-April 2021. The COVID-19 vaccines have been determined by the FDA to be safe and effective and are being thoughtfully distributed in phases.
Americas Health Insurance Plans is calling on more government support to cover the cost of COVID-19 tests which it says could be between 6 billion and. Fear of COVID-19 alone is unlikely to trigger business interruption insurance coverage. Insurers are legally required to pay for in-network testing so try to find a medical facility where you know youll be covered.
The COVID-19 vaccine will be provided by the federal government at no cost to providers. What Travel Insurance Does Not Cover Related to COVID-19. Does my business interruption insurance policy cover my business if my employees stay home out of concern about COVID-19.
In most cases there should be no out-of-pocket costs such as co-pays or deductibles for these tests. However it is expected that providers will charge a vaccine administration fee. Does my Ambetter plan cover testing and screening services for COVID-19.
Standard travel insurance does not cover trip cancellation due to fears or concerns about traveling during the coronavirus pandemic or any other epidemic. Loren Adler and Christen Linke Young examine the existing coverage for COVID-19 testing outline ways to improve access and propose how to better finance COVID-19 testing in the future. Some plans cover COVID-19 like any other new illness while others might have more specifications.
Once your deductible has been met only standard copays will apply. Travel medical insurance plans can help cover costs associated with the following situations. All member cost share copayment coinsurance andor deductible amounts will be waived for COVID-19 screening visits and if billed alongside a COVID-19 testing code.
When medically necessary diagnostic testing or medical screening services are ordered andor referred by a licensed health care provider your Ambetter plan will cover the cost of medically necessary COVID-19.

Coronavirus Information Ambetter From Superior Healthplan
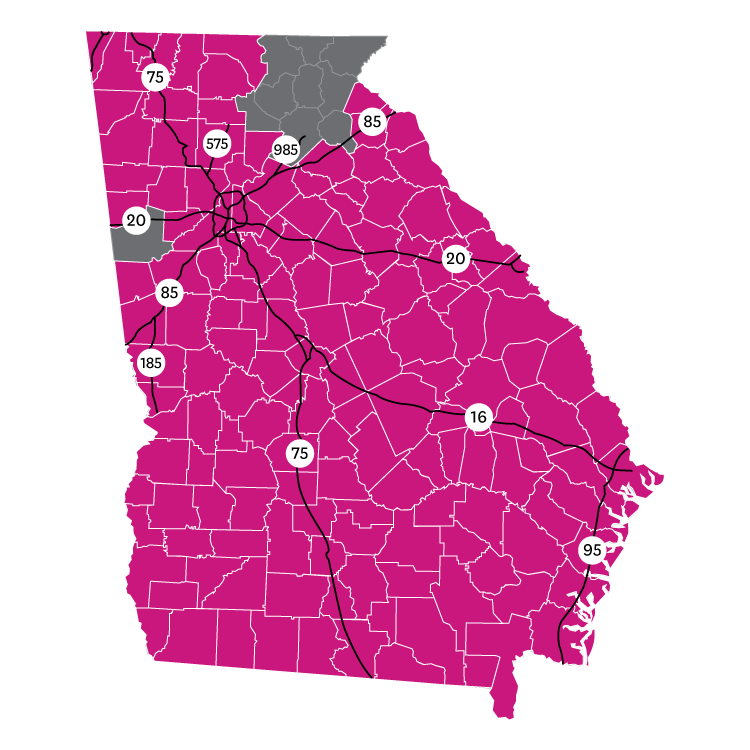
Ambetter Georgia Coverage Map Ambetter From Peach State Health Plan

Mississippi Department Of Health Covid 19 Testing Sites

April18 Cvs Minute Clinics Article
Ambetter Health Posts Facebook
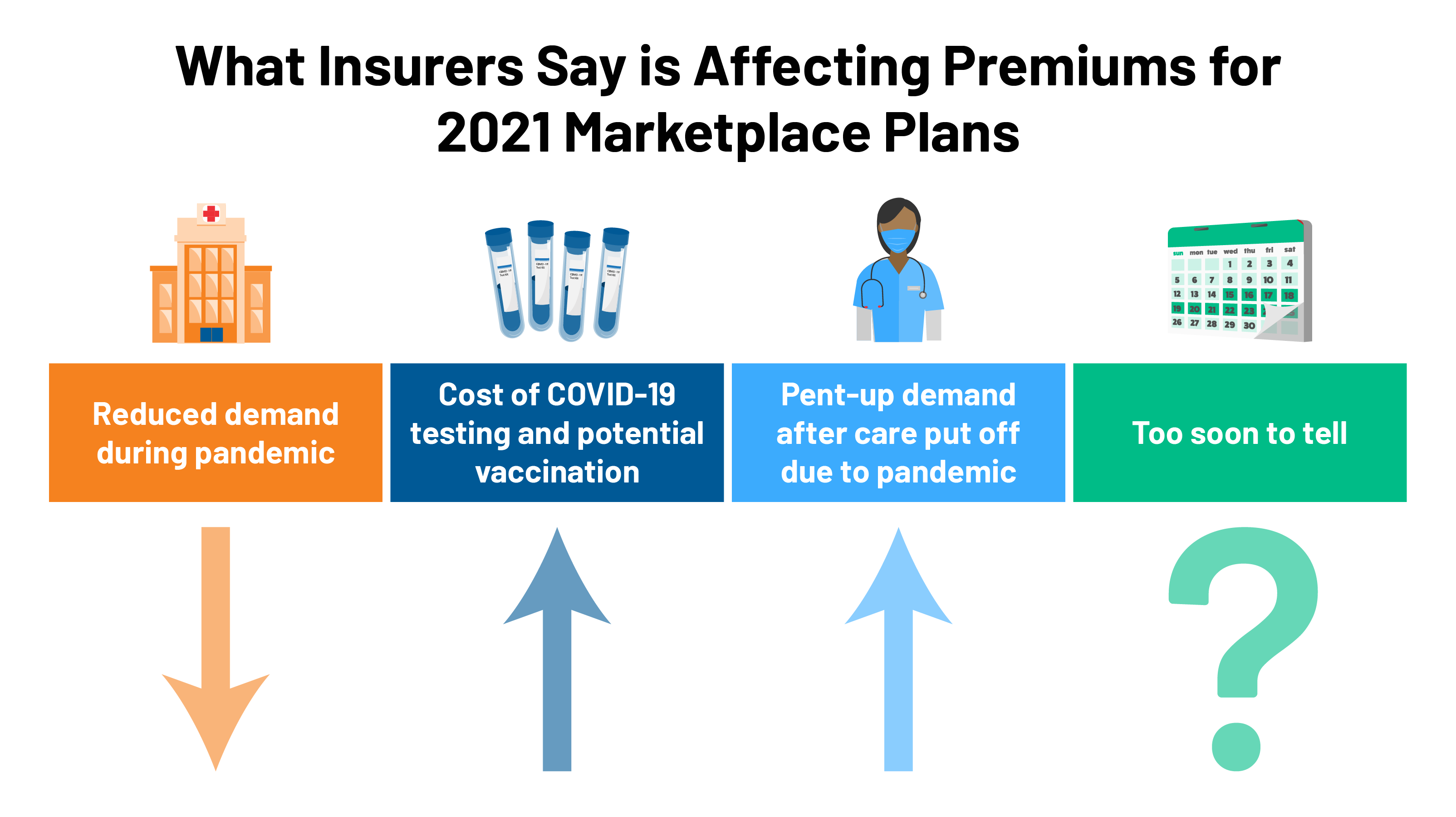
2021 Premium Changes On Aca Exchanges And The Impact Of Covid 19 On Rates Kff
![]()
Coronavirus Coverage Ambetter From Coordinated Care

Ambetter Coordinated Care Cpap Coverage Health Sqyre
Ambetter Health Posts Facebook

Qualchoice Health Insurance Brokers
Ambetter Health Posts Facebook
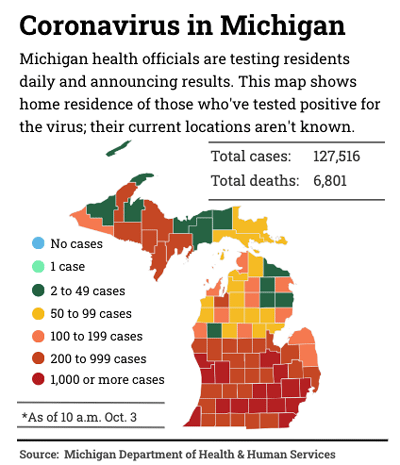
Covid 19 Update Michigan Residents Will Have Access To Ambetter Health Insurance Adient Sells Automotive Fabrics Business And More Dbusiness Magazine
Ambetter Health Posts Facebook

Coronavirus Guidelines Ambetter Of Illinois

Covid 19 Guidance For Providers Ambetter From Sunshine Health

Coronavirus Information Ambetter From Superior Healthplan



Posting Komentar untuk "Does My Insurance Cover Covid Testing Ambetter"