Does Unitedhealth Cover Rapid Covid Testing
A wide variety of different states but most of the states are in that 9-15 range. Find COVID-19 coverage information and learn how to access resources and support.
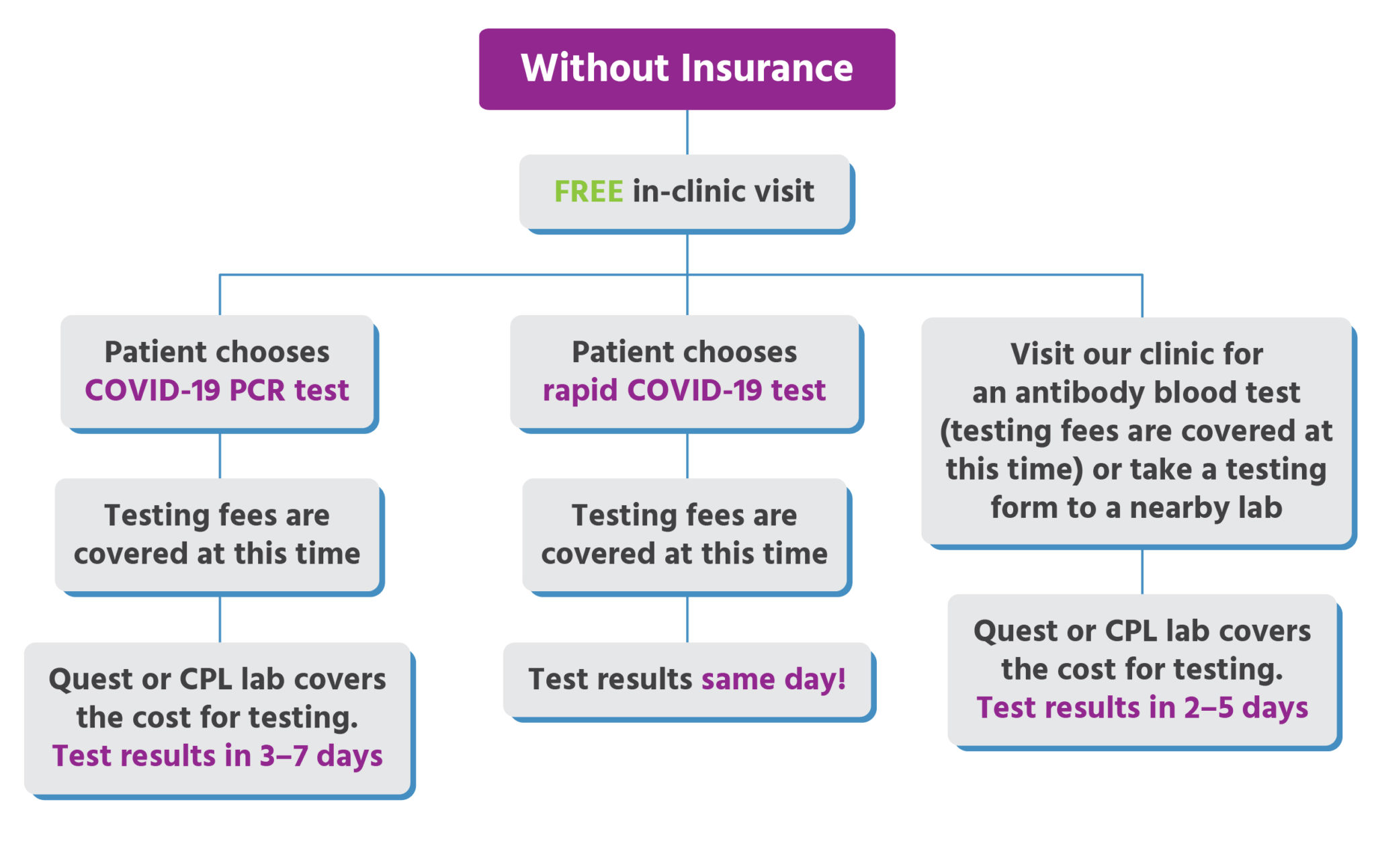
Urgent Care For Kids Insurance Accepted Cost
This means the members will have no deductible or coinsurance for the actual test.

Does unitedhealth cover rapid covid testing. UnitedHealthcare will cover FDA-authorized rapid point of care virusantigen detection and antibody testing. Department of Health and Human Services HHS provides claims reimbursement to health care providers generally at Medicare rates for testing uninsured individuals for COVID-19 treating uninsured individuals with a COVID-19 diagnosis and administering COVID-19 vaccines to uninsured individuals. Genetic or molecular tests antigen tests and antibody tests.
Learn about COVID-19 testing and treatment coverage. This is the people that have been diagnosed through a test or diagnosis with COVID and overall across the United States about 10- 105 of the population has been diagnosed with COVID. Its very important that if you test positive for Coronavirus COVID-19 that you are treated as soon as possible.
May not seek any reimbursement including through balance billing from the vaccine recipient. Therefore any money collected from the individual must be returned to the individual if the provider received funding for that patient through this program. UnitedHealthcare health plans do not cover COVID-19 surveillance testing which is testing used for public health or social purposes such as employment return to workplace education travel or entertainment.
This will apply to PEIA PPB plans A B C and D. If your doctor or other health care professional provides a prescription or order for the over-the-counter COVID-19 test as part of clinical care you may submit a claim for reimbursement with both the prescription and detailed receipt to UnitedHealthcare. Effective March 26 2021 UnitedHealthcare will reimburse COVID-19 testing for urgent care facilities only when billed with a COVID-19 testing procedure code along with one of the appropriate Z codes Z20828 Z03818 andor Z20822.
UnitedHealthcare will reimburse out-of-network providers for COVID-19 testing-related visits and COVID-19 related treatment or services according to the rates outlined in the Medicaid Fee Schedule. March 31 2020 - UnitedHealth Group Research Development and OptumCare clinicians have determined that self-administered COVID-19 tests are as effective as provider. UnitedHealthcare will cover medically appropriate COVID-19 testing at no cost share during the national public health emergency period currently scheduled to end Oct.
In our new world connection is critical and Optum is here to help. Talk to a provider using virtual visits. REQUEST A HOME TESTING KIT This COVID-19 treatment policy applies to customers in the United States who are covered under Cignas employer-union-sponsored insured group health plans insured plans for US-based.
HRSA COVID-19 Coverage Assistance Fund for vaccine recipients whose insurance does not cover vaccine administration fees or does but typically has cost-sharing. The program reimburses providers for COVID-19 testing treatment or vaccine administration fees for uninsured individuals. You should get tested as soon as possible.
Loren Adler and Christen Linke Young examine the existing coverage for COVID-19 testing outline ways to improve access and propose how to better finance COVID-19 testing in the future. Medicaid will cover the full cost of COVID-19 testing for the uninsured as directed by the CARES Act. Effective with date of service 2042020 and after PEIA will cover COVID-19 testing at a network provider at 100 of the contracted allowance for members who meet CDC guidelines for testing.
Theres a new cheap and rapid COVID-19 test in our arsenal thanks to an emergency use authorization from the Food and Drug Administration FDA. This map shows locations where COVID-19 testing is available. By Kelsey Waddill.
Swabs taken from the nostril and mid-nose of COVID-19 patients picked up the disease in more than 90 percent of cases according to healthcare company UnitedHealth Group which created the test. If they are full try another location. To help with this UnitedHealthcare is waiving member cost-sharing for the treatment of COVID-19 based on confirmed positive diagnosis through the national public health emergecy period for Medicare Advantage Medicaid Individual and Group Market fully insured health.
Rapid Point of Care Testing. Test results are available within 24 hours or less of your visit. As such regardless of insurance status providers cannot charge patients for the COVID-19.
You may be able to set up a telehealth visit to talk to a provider from your home both for routine medical care and for care related to COVID. This means that most patients will receive their test. Testing for return to work or school travel or other recreational activities is not covered by your plan.
See COVID-19 stories of compassion collaboration and innovation for the. UnitedHealthcare is also waiving cost sharing for COVID-19 testing-related services received in-person or via telehealth for the following health plans. These tests are only covered when required by applicable law and adjudicated in accordance with the members benefit plan.
There are three types of COVID-19 tests. An increase in rapid testing could help stop the spread of COVID-19. EmblemHealth continues to cover medically appropriate FDA-authorized COVID-19 tests if your doctor thinks you may have COVID-19 or you were exposed to COVID-19 and orders the test.
Its where youll find stories of courage compassion and connection that define this moment. The Community Circle is our way to educate inspire and bring all of us together in the fight against COVID-19. Testing requirements and availability can vary by location.
The COVID-19 testing location you want to use may be busy and may take a few days to get an appointment. You can now make an appointment for a free rapid COVID-19 virus test at the Health Departments COVID Express sites throughout the city. Cigna is waiving out-of-pocket costs for FDA-approved COVID-19 diagnostic PCR and antigen testing tests as required by the CARES Act.
State variations and regulations may apply. 17 2021 when ordered by a.

Could A Rapid Neutralising Antibody Test Free Up Doses Of Covid 19 Vaccines For Low And Middle Income Countries Gavi The Vaccine Alliance

Roche Diagram The Future Of Health Systems And Their Role In Accelerating Pandemic Resilience

How Much Do We Know About Countries Preparedness To Respond To Pandemics Insights From Two Country Level Indices

Coding Submissions Reimbursement Uhcprovider Com

Covid 19 Testing Gohealth Urgent Care

Universal Health Coverage Uhc And The Coronavirus Crisis Challenges And Responses Maintaining Essential Health Services While Responding To Covid 19 Socialprotection Org

How Home Coronavirus Testing Could Slow Disease Spread

Covid 19 Testing Bills Surprise New Yorkers Modern Healthcare

Telehealth And Covid 19 Billing And Coding Resources

List Of Retailers Offering Coronavirus Testing
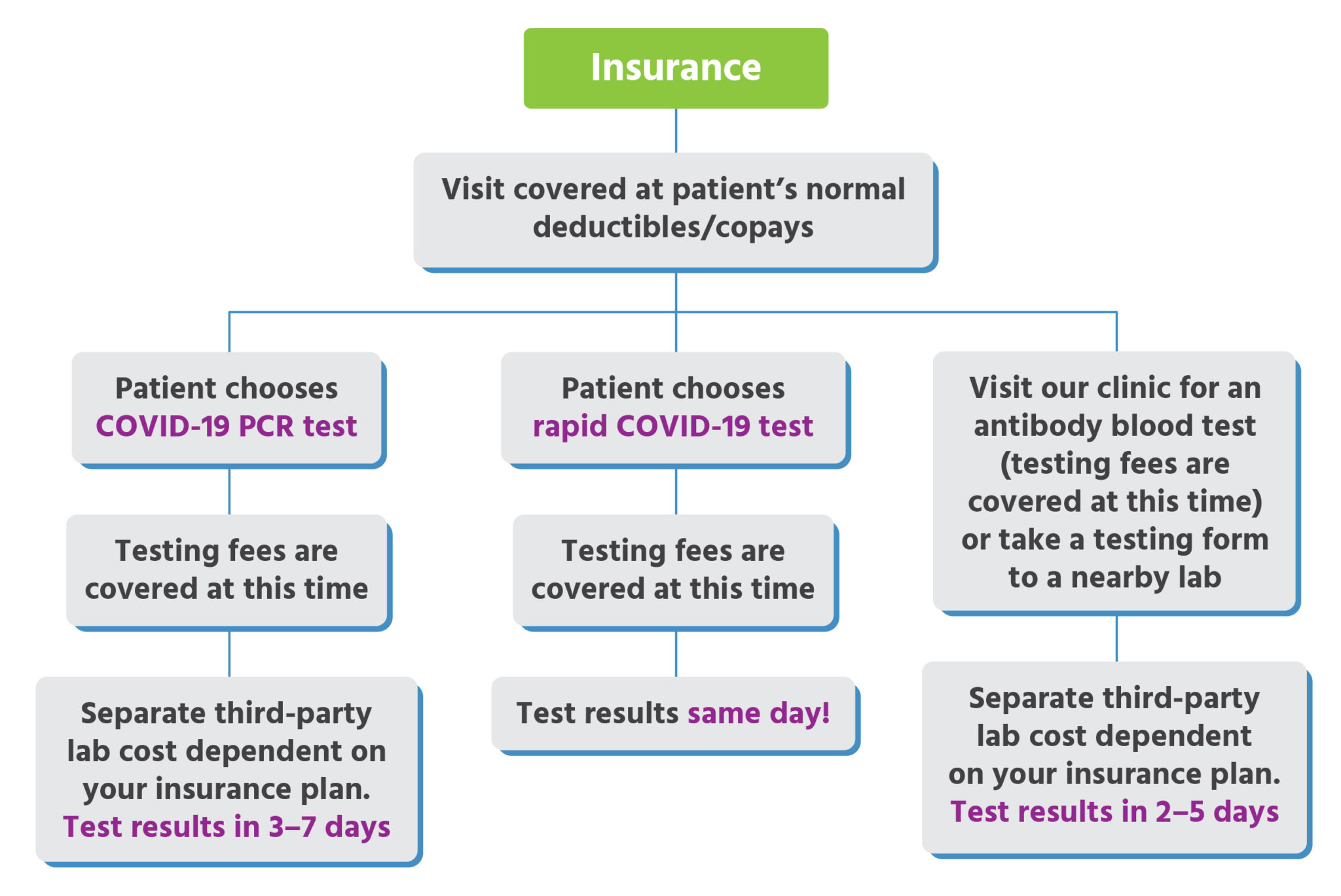
Urgent Care For Kids Insurance Accepted Cost

Unitedhealthcare Has Waived All Diagnostic Test Cost Sharing For Insured Members For Covid 19 Testing Healthcare Purchasing News

Antigen Rapid Tests Country Implementation Support Find

False Negative How Long Does It Take For Coronavirus To Become Detectable By Pcr Gavi The Vaccine Alliance

What Is A Pcr Covid Test Bioreference Laboratories

Covid 19 Testing Healthcare Services In New York Multi Specialty Practices

Coverage And Resources For Covid 19 Unitedhealthcare Community Plan Medicare Medicaid Health Plans


Posting Komentar untuk "Does Unitedhealth Cover Rapid Covid Testing"