Does Insurance Cover Covid Antigen Test
Per guidance from the Centers for Medicare Medicaid Services CMS the Department of Labor and the Department of the Treasury all Commercial Medicaid and Medicare plans must cover COVID-19. A doctor must order a COVID-19 test for you.

Pcr Test In Puerto Vallarta Available In Three Locations Hospital Cmq
How much is a COVID-19 test SUPPOSED to cost.

Does insurance cover covid antigen test. Cigna Health and Life Insurance Company Connecticut General Life Insurance Company or their affiliates. Medicare Part B Medical Insurance covers a COVID-19 antibody or serology test. Whether or not you have symptoms of COVID-19.
Rapid tests take under 15 minutes to detect covid by pinpointing proteins called antigens. Find a COVID-19 testing location near you by using this tool. If you or your child has ever had a rapid strep test youve had firsthand experience with an antigen test.
Tests to diagnose or aid the diagnosis of COVID-19. When tests are available for you in your state Medicare covers and you pay nothing for. Antibody tests are useful right now from a public health perspective to determine what percentage of a population has been exposed to the new coronavirus.
Additionally many test sites in the Commonwealth test uninsured individuals for free. Though many airlines including Air Canada and WestJet and insurance companies like Manulife Allianz and Blue Cross are already offering COVID-19 coverage these plans generally do not cover. Lauderdale West Palm Beach and Miami.
Youll notice several major chains on the list of where to get a COVID-19 test including CVS Walgreens and Rite AidAll of these often offer PCR testing at no additional cost if using insurance or if you fall under some federal programs for those without insurance. They may be less meaningful on an individual level. PCR tests require expensive and specialized equipment and can take hours or days to get results.
Testing is free with insurance plus a 35 charge for next-day results or 75 for same-day results. All Anthem plans cover medically necessary COVID-19 testing and the care visit where the test takes place with no out-of-pocket costs. Cigna covers the cost of administering FDA-authorized COVID-19 vaccines at 100 without any out-of-pocket costs when performed by an in-network or out-of-network provider.
Going forward insurance plans will no longer be able to use medical necessity as a standard for coverage and will instead be required to cover all. Not all tests are covered by insurance but since the passage of the Families First Coronavirus Response Act in March many people should have coverage for coronavirus testing. COVID-19 testing for symptomatic individuals and close contacts is usually covered by insurance and available at no cost to you.
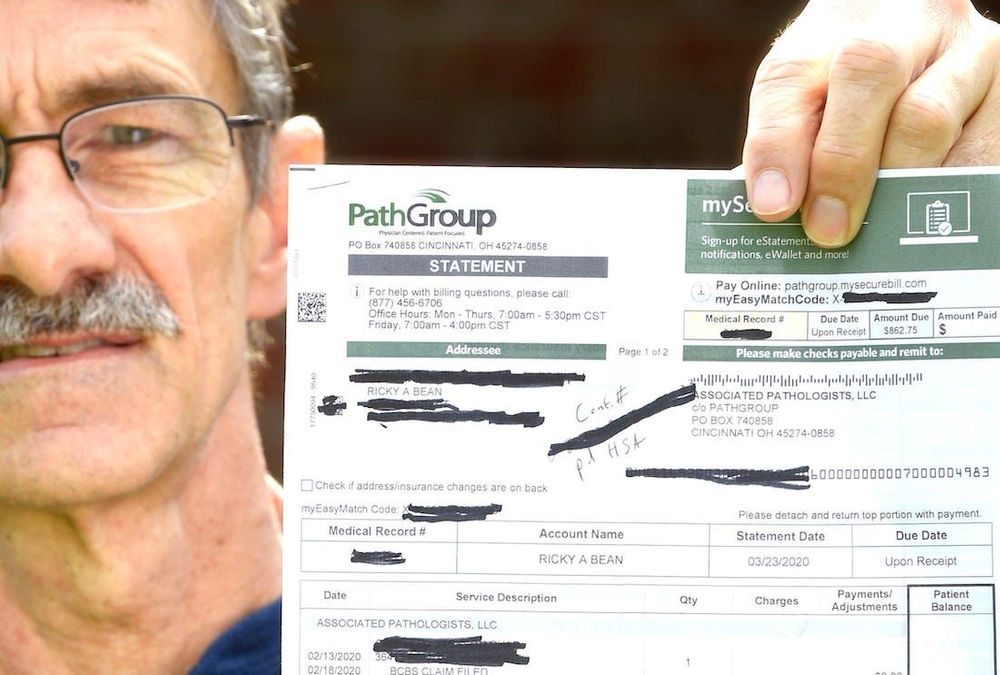
Like other types of medical fees insurance companies have to negotiate the cost with the providers and labs that dole out the tests. To receive your test results you will need to sign in or create a Labcorp Patient account. A tests accuracy depends on a number of factors including its quality and the location of the person tested.
What do I do if my test is positive. If youre in a location without many COVID-19 testing sites you may want to head to your neighborhood drugstore. Find vaccine information and resources in your state COVID-19 Vaccines Care and Coverage.
Worksite Labs conducts tests in Ft. So to sum it up you should not have to pay anything for a COVID-19 test if you have Medicare Part B. Per guidance from the Centers for Medicare Medicaid Services CMS the Department of Labor and the Department of the Treasury all Commercial Medicaid and Medicare plans must cover COVID-19 serological antibody testing with no cost-sharing.
The requirement also applies to self-insured plans. Lastly Medicare Part B will also provide full coverage of COVID-19 antibody tests which help determine if an individual has already been infected by the virus and developed immunity. Medicare covers these tests at different locations including some parking lot test sites.
Vaccine guidelines and requirements can vary by state and county. The tests are similar to a pregnancy test with one or two lines displayed depending on the result. The cost is 90 for results in 24 hours or 150 for results in 12 hours.
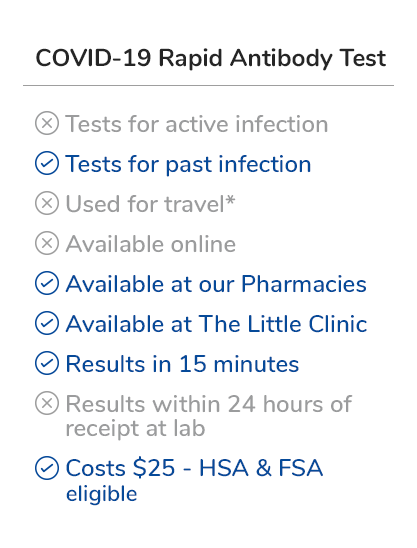
Covid Testing LLC does testing at several locations in Orlando and Central Florida. In contrast antigen tests. What it is This FDA-authorized test helps see if youve developed an immune response and may not be at immediate risk of.
Congress required health plans to fully cover COVID-19 testing but insurance companies are starting to argue they should only have to pay if patients show symptoms or tests are ordered by a. If you are uninsured please call your local test site to confirm before making an appointment. Most health insurance plans do not cover COVID-19 tests for reasons other than diagnosis or treatment by a health care professional.
Your primary care provider may be willing to test you for COVID-19 if you dont have symptoms although your insurance may not cover the test. Please talk to a doctor first to be certain you need a COVID-19 test. While other diagnostic tests for COVID-19 known as PCR tests look for genetic material from the virus the antigen test looks for molecules on the surface of the virus.
COVID-19 testing is available at no cost. The requirement also applies to self-insured plans. Some tests for related respiratory conditions to aid diagnosis of COVID-19 done together with the COVID-19 test.
Prices for coronavirus testing arent federally regulated according to a report from The Peterson Center on Healthcare and the Kaiser Family Foundation Peterson-KFF. Your costs in Original Medicare You pay nothing for this test. Food and Drug Administration FDA approved COVID-19 home tests that you buy at a pharmacy or store without a prescription or order from a licensed health care professional are not covered by your plan.
This COVID-19 treatment policy applies to customers in the United States who are covered under Cignas employer-union-sponsored insured group health plans insured plans for US-based. Labcorp will bill the cost of the COVID-19 antibody test directly to your health plan if you are insured or if you are uninsured Labcorp will bill the appropriate government program. The 10 service fee is not submitted to insurance for reimbursement.
See below for those not covered This means you do not need to pay out-of-pocket costs copay coinsurance or deductible for tests that are provided or ordered by a healthcare provider. Blue Shield and Blue Shield Promise cover most diagnostic tests for individuals at no out-of-pocket cost to you.
Pharmacy Hours Online Services Coronavirus Updates Kroger

Covid Antigen Test In Puerto Vallarta Now Available At Cmq Hospitals
Covid 19 Testing Where To Go When To Get Tested In Time For The Holidays In The San Francisco Bay Area Abc7 San Francisco

Coronavirus Test In Puerto Vallarta Hospital Cmq
Faqs On Medicare Coverage And Costs Related To Covid 19 Testing And Treatment Kff
.jpg)
Covid 19 Pcr And Antigen Tests Los Cabos

Testing For Covid 19 Faqs Blue Shield Of Ca

Covid 19 Igm Igg Antibody Rapid Test Results In 10 Minutes

Drive Thru Covid 19 Testing Clinic Near Me Covid Clinic
How Much Does A Rapid Covid 19 Test Cost Without Insurance Mira

Covid Antigen Test In Puerto Vallarta Now Available At Cmq Hospitals
![]()
Covid 19 Test Prices And Payment Policy Peterson Kff Health System Tracker

How Americans Can Get A Covid Test In Mexico The Washington Post

Covid 19 Testing Healthcare Services In New York Multi Specialty Practices

Coronavirus Faq For Wellfleet Student Members Wellfleet Student

Covid Antigen Test In Puerto Vallarta Now Available At Cmq Hospitals

Binaxnow Covid 19 Antigen Self Test
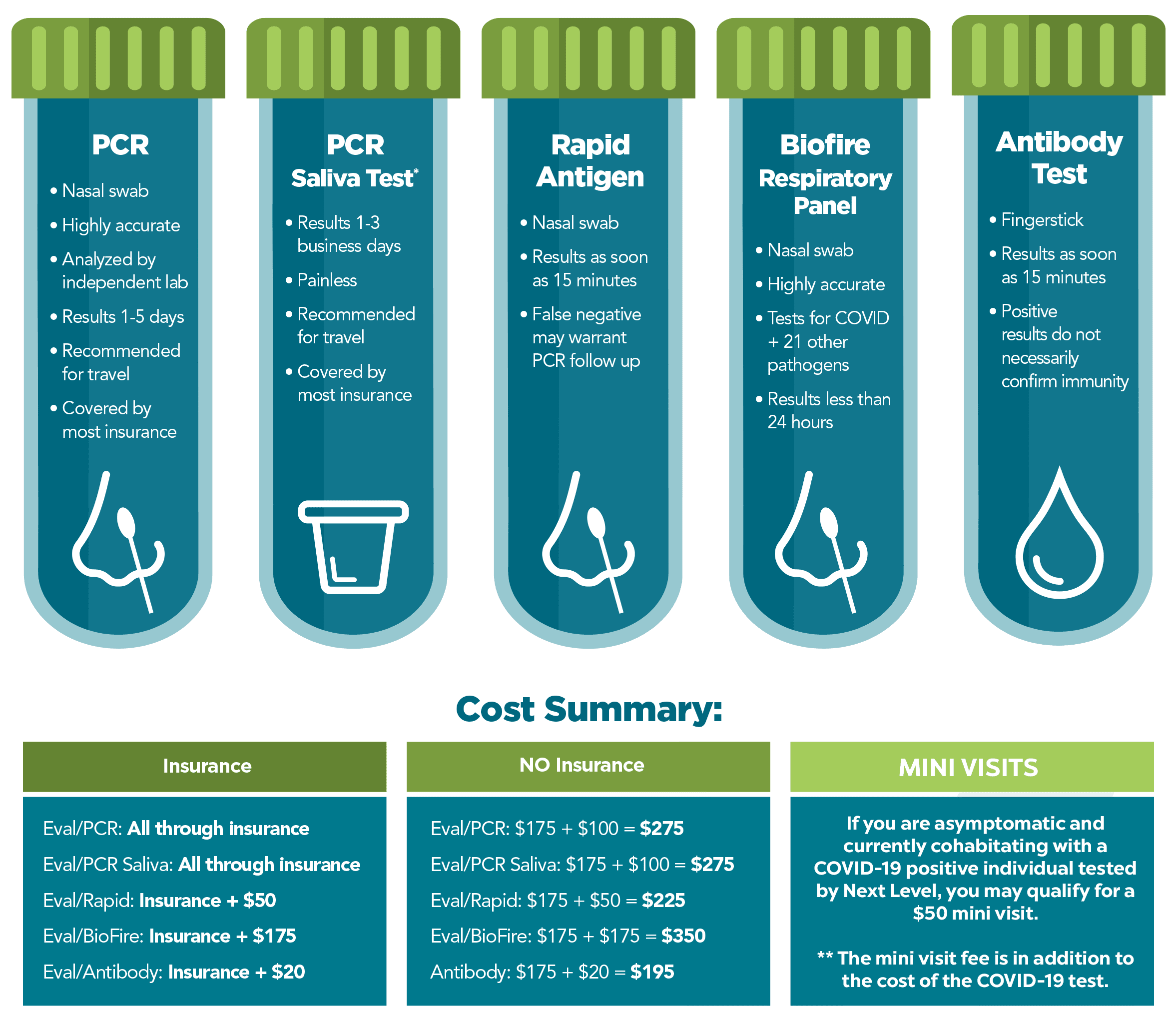
Covid 19 Testing Next Level Urgent Care
Posting Komentar untuk "Does Insurance Cover Covid Antigen Test"