Does My Cigna Insurance Cover Covid Testing
Congress required health plans to fully cover COVID-19 testing but insurance companies are starting to argue they should only have to pay if patients show symptoms or tests are ordered by a. Cigna is waiving out-of-pocket costs for office visits related to testing and diagnostic tests for COVID-19 as required by the CARES Act.

Centro De Recursos Sobre El Coronavirus Covid 19 Cigna
One type looks for genetic material from the virus.

Does my cigna insurance cover covid testing. Or public health surveillance and antibody tests are not covered by Cignas standard coverage but may be covered as required by state law. Diagnostic testing for COVID-19 molecular or antigen diagnostic tests including rapid tests saliva tests etc is covered without cost-share prior authorization or other medical management requirements through October 17 2021. Many insurers youve seen in the news like Blue Cross Blue Shield Aetna and Cigna have announced that if you or someone in your family gets COVID-19 you wont have to pay anything out of pocket.
Get more information on how to get tested at a center or at home. Cigna is waiving out-of-pocket costs for COVID-19 FDA-approved testing through the PHE period currently scheduled to end on October 18 2021. Does my insurance cover COVID-19 testing and treatment.
Will Cigna cover my medical care if I contract COVID-19. Cigna is waiving out-of-pocket costs for COVID-19 visits with in-network providers whether at a providers office urgent care center emergency room or via virtual care through the Public Health Emergency PHE period currently scheduled to end on October 18 2021. BLOOMFIELD Conn March 5 2020 PRNewswire -- Cigna NYSE.
Another type looks for proteins on the virus. BLOOMFIELD Conn March 5 2020 PRNewswire -- Cigna NYSE. 5 Locations for diagnostic screening and testing.
This is usually called polymerase chain reaction PCR. New Cigna Care Card to Help Clients Provide Financial Assistance to Employees Impacted By COVID-19. Cigna is facing a lawsuit arguing it failed to pay a New Jersey medical office for COVID-19 diagnostic testing and treatment according to a complaint filed this week in federal court.
Cigna is waiving out-of-pocket costs for FDA-approved COVID-19 diagnostic PCR and antigen testing tests. CI customers will have access to coronavirus COVID-19 testing as prescribed by health practitioners and the company will waive all co-pays or cost-shares to help fight the rapid spread of the virus in the. Published on March 10 2020 March 10 2020 28 Likes 2 Comments.
Cigna covers out-of-pocket expenses for a covered COVID-19 diagnostic visit and testing with no customer cost share through the Public Health Emergency PHE period currently scheduled to end on October 18 2021. There are different types of viral tests. CI customers will have access to coronavirus COVID-19 testing as prescribed by health practitioners and the company will waive.
How is Cigna covering COVID-19 testing. Cigna Health does not specify a limit on the number of COVID-19 tests it. The medicare reimburse rate for a nasal swab COVID test is a 100 dollars but theres no law that caps what a private facility can charge an insurance company.
Results are available in 1-3 days after sample is received at lab. Under the terms of the Families First Coronavirus Response Act HR6201 Medicare Medicaid and private health insurance plans including grandfathered plans are required to fully cover the cost of COVID-19 testing without any cost-sharing or prior-authorization requirements for the duration of the emergency period which has most recently been extended through mid-April 2021. The test looks for the virus in your breathing passages.
Cigna covers medical care for COVID-19 treatment subject to standard cost share copay and deductibles. Does Cigna Cover Covid testing at urgent care. Viral Test for COVID-19 Cigna.
Cigna covers medical care for COVID-19 treatment subject to standard cost share copay and deductibles. Cigna Launches Real-Time Digital. According to its website Cigna is waiving out-of-pocket costs for COVID-19 FDA-approved testing through Jan.
A COVID-19 viral test is a way to find out if you have COVID-19. Cigna Expands and Extends COVID-19 Relief Efforts for Medicare Advantage and Individual and Family Plans. Cigna Covers Cost Of Coronavirus Tests For Customers.

Most People Won T Have To Pay For Covid 19 Testing Coronavirus

Covid 19 Pruebas Tratamiento Y Cobertura De La Vacuna Cigna
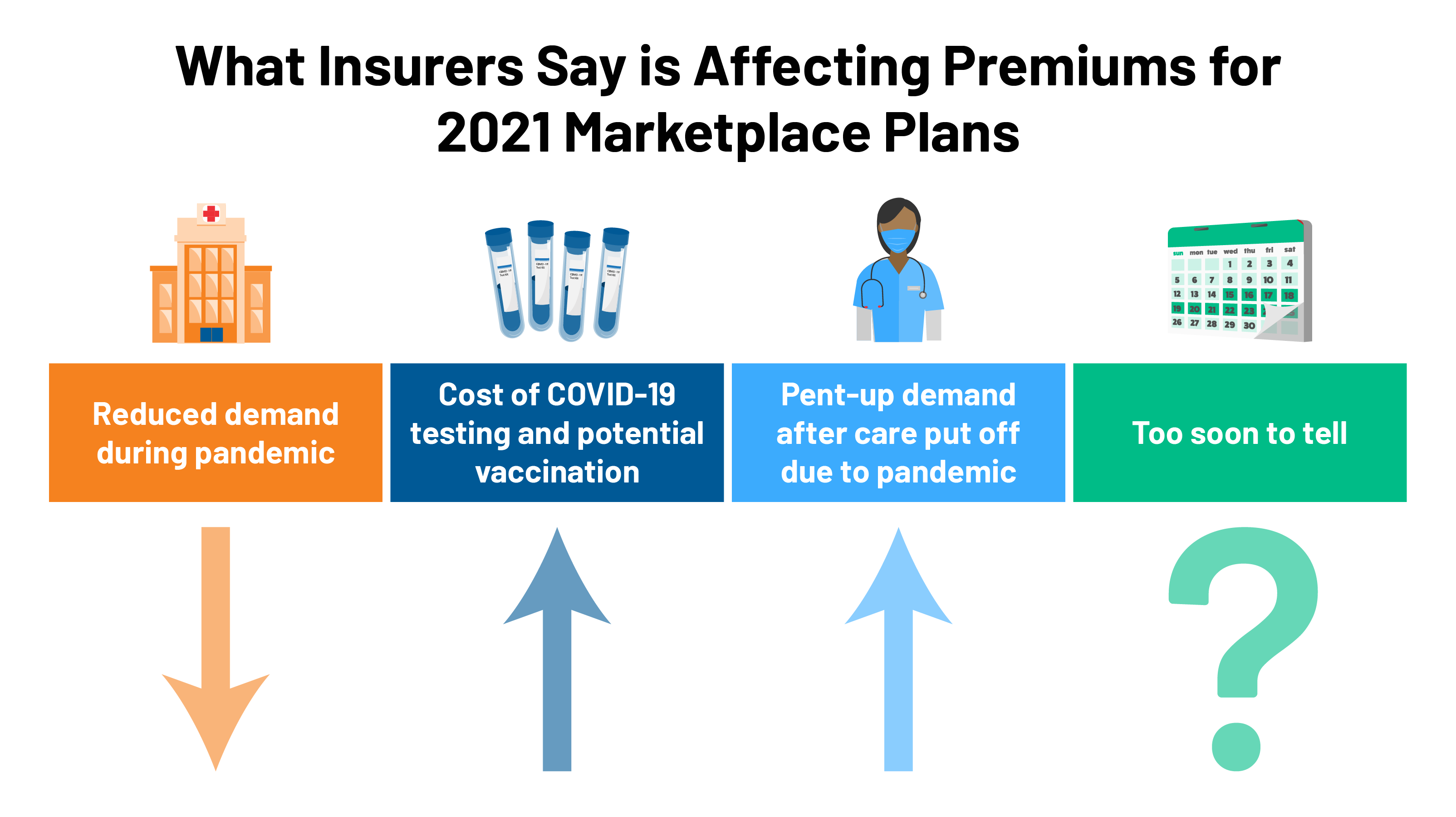
2021 Premium Changes On Aca Exchanges And The Impact Of Covid 19 On Rates Kff

Cigna Requires Employees Returning To Office To Be Fully Vaccinated Reuters

Cigna And Humana Waive Coronavirus Treatment Costs

Does Your Health Insurance Cover You For Covid 19 Cbs News
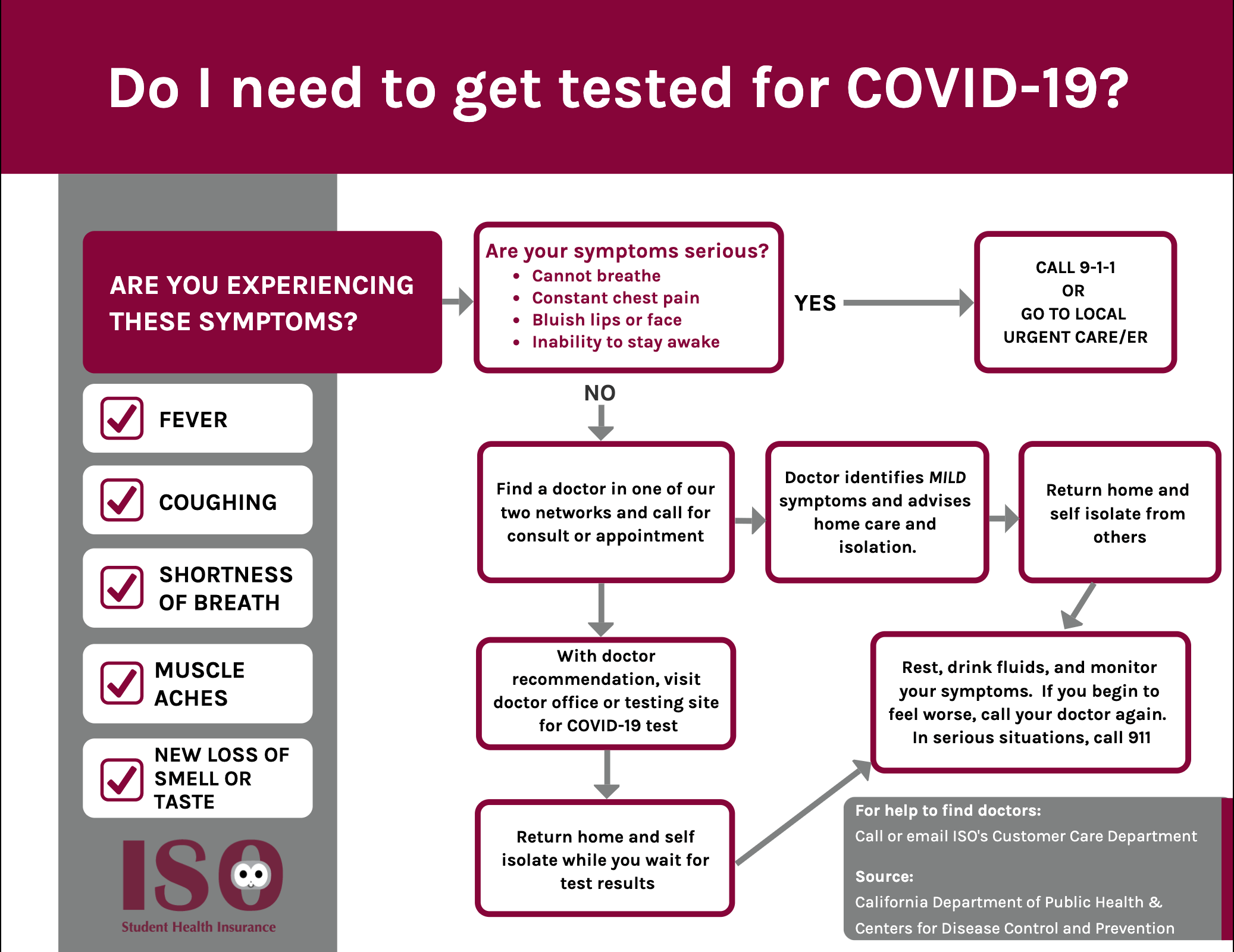
Iso International Student Insurance

Pcr Test In Puerto Vallarta Available In Three Locations Hospital Cmq
Covid Catch 22 They Got A Big Er Bill Because Hospitals Couldn T Test For Virus Kaiser Health News

Centro De Recursos Sobre El Coronavirus Covid 19 Cigna

Centro De Recursos Sobre El Coronavirus Covid 19 Cigna

What To Know About Coronavirus Your Insurance Utah Insurance Department

Coronavirus Faq For Wellfleet Student Members Wellfleet Student
Posting Komentar untuk "Does My Cigna Insurance Cover Covid Testing"