Cigna Health Insurance Cover Covid Testing
BLOOMFIELD Conn March 5 2020 PRNewswire -- Cigna NYSE. Insurance companies like Cigna and Aetna said they will waive copays for testing and cover treatment.

Cigna Requires Employees Returning To Office To Be Fully Vaccinated Reuters
New Cigna Care Card to Help Clients Provide Financial Assistance to Employees Impacted By COVID-19.

Cigna health insurance cover covid testing. Results are available in 1-3 days after sample is received at lab. Self-initiated at-home specimen collection kits that are FDA-approved such as the Pixel by LabCorp testing kit will be covered by Cigna cost share waived. The test is most often done on a sample from the nose throat or lungs.
Provide your Cigna insurance information. Has COVID-19 affected the Aetna health insurance as well as the Hartford Life Insurance. Cigna Expands and Extends COVID-19 Relief Efforts for Medicare Advantage and Individual and Family Plans.
It looks for evidence of the virus in your breathing passages or lungs respiratory system. Cigna Health and Life Insurance Co. Requires telemedicine appointment before scheduling NAA COVID Test.
Medical benefits and coverage under Aetna and life insurance have not changed. Cigna is facing a lawsuit arguing it failed to pay a New Jersey medical office for COVID-19 diagnostic testing and treatment according to a complaint filed this week in federal court. The Free Cigna COVID-19 Income Protection Benefit is offered by Cigna Worldwide General Insurance Company Limited Cigna the Company we our or us and is subject to the following terms conditions and exclusions.
Complete an online screening. Effective immediately Cigna will waive customers out-of-pocket costs for COVID-19 testing-related visits with in-network providers whether at a doctors office urgent care clinic emergency room or via telehealth through May 31 2020. Cigna Launches Real-Time Digital.
Medicaid patients may not pay out of pocket for Rapid COVID Testing. Or public health surveillance and antibody tests are not covered by Cignas standard coverage but may be covered as required by state law. Cigna increased the weighting factor of the assigned Medicare DRG by 20 for members hospitalized with a COVID-19 diagnosis and discharged during the COVID-19 Public Health Emergency PHE period.
Its sometimes done on a sample of saliva. November 6 2020. Cigna covers medical care for COVID-19 treatment subject to standard cost share copay and deductibles.
Cigna will determine coverage for each test based on the specific codes that the. Medicare and Medicaid are also covering those costs. This may also be called a PCR test or antigen test.
A complaint was filed today against Cigna Health and Life Insurance by Murphy Medical Associates regarding the provision of COVID-19 testing in the state of Connecticut. Cigna is waiving out-of-pocket costs for office visits related to testing and diagnostic tests for COVID-19 as required by the CARES Act. The company will not require prior authorization prior certification prior notification or step therapy protocols for these services.
In Vitro Diagnostic Testing coverage policy for additional coverage criteria. Testing capacity in the US is still limited. Cigna Refused To Cover COVID-19 Testing Practice Says.
CI customers will have access to coronavirus COVID-19 testing as prescribed by health. As previously announced Cigna will cover the diagnostic test with no cost-sharing when recommended by a health care professional. COVID-19 is diagnosed with a viral test.
COVID-19 LABORATORY TESTING Q. And for its globally mobile customers. Will Cigna cover the laboratory test for COVID-19.
BLOOMFIELD Conn March 5 2020 PRNewswire -- Cigna NYSE. Centene will cover COVID-19 testing and screening services for Medicaid Medicare and Marketplace members and is waiving all associated member cost share amounts for COVID-19 testing and screening. Cigna covers out-of-pocket expenses for a covered COVID-19 diagnostic visit and testing with no customer cost share through the Public Health Emergency PHE period currently scheduled to end on October 18 2021.
In all cases providers should bill the COVID-19 test with the diagnosis code that is appropriate for the reason for the test. Please review our COVID-19. If so in which ways.
Generally all patients are entitled to receive a no cost NAA Covid-19 Test NOT RAPID TEST following a no cost telemedicine consultation as most insurance companies have waived all deductible and copay costs Additionally if you are uninsured upon signing an attestation the federal government will cover your costs for a NAA COVID-19 Test. Wrongly refused to reimburse more than 46 million in Covid-19 testing costs on behalf of more than 4400 patients a Connecticut medical practice alleged Friday in a federal lawsuit. Generally only NAA Test is covered under these health insurance plans.
The health insurers have also waived prior authorization requirements for Covid-19 testing and treatments as well as hospital transfers to post-acute care facilities during the epidemic in order. Plans and issuers are not required to provide coverage for this type of COVID-19 testing. The case is Murphy Medical Associates LLC et al.
Under the terms of the Families First Coronavirus Response Act HR6201 Medicare Medicaid and private health insurance plans including grandfathered plans are required to fully cover the cost of COVID-19 testing without any cost-sharing or prior-authorization requirements for the duration of the emergency period which has most recently been extended through mid-April 2021. Cigna Owes Millions in Covid Testing Costs Doctor Group Claims 1 Cigna Health Life Insurance Co. Generally Rapid COVID-19 testing is not covered but standard NAA testing is usually covered.
CI customers will have access to coronavirus COVID-19 testing as prescribed by health practitioners and the company will waive all co-pays or cost-shares to help fight the rapid spread of the virus in the US.

Centro De Recursos Sobre El Coronavirus Covid 19 Cigna

Covid 19 Pruebas Tratamiento Y Cobertura De La Vacuna Cigna

Centro De Recursos Sobre El Coronavirus Covid 19 Cigna

Centro De Recursos Sobre El Coronavirus Covid 19 Cigna
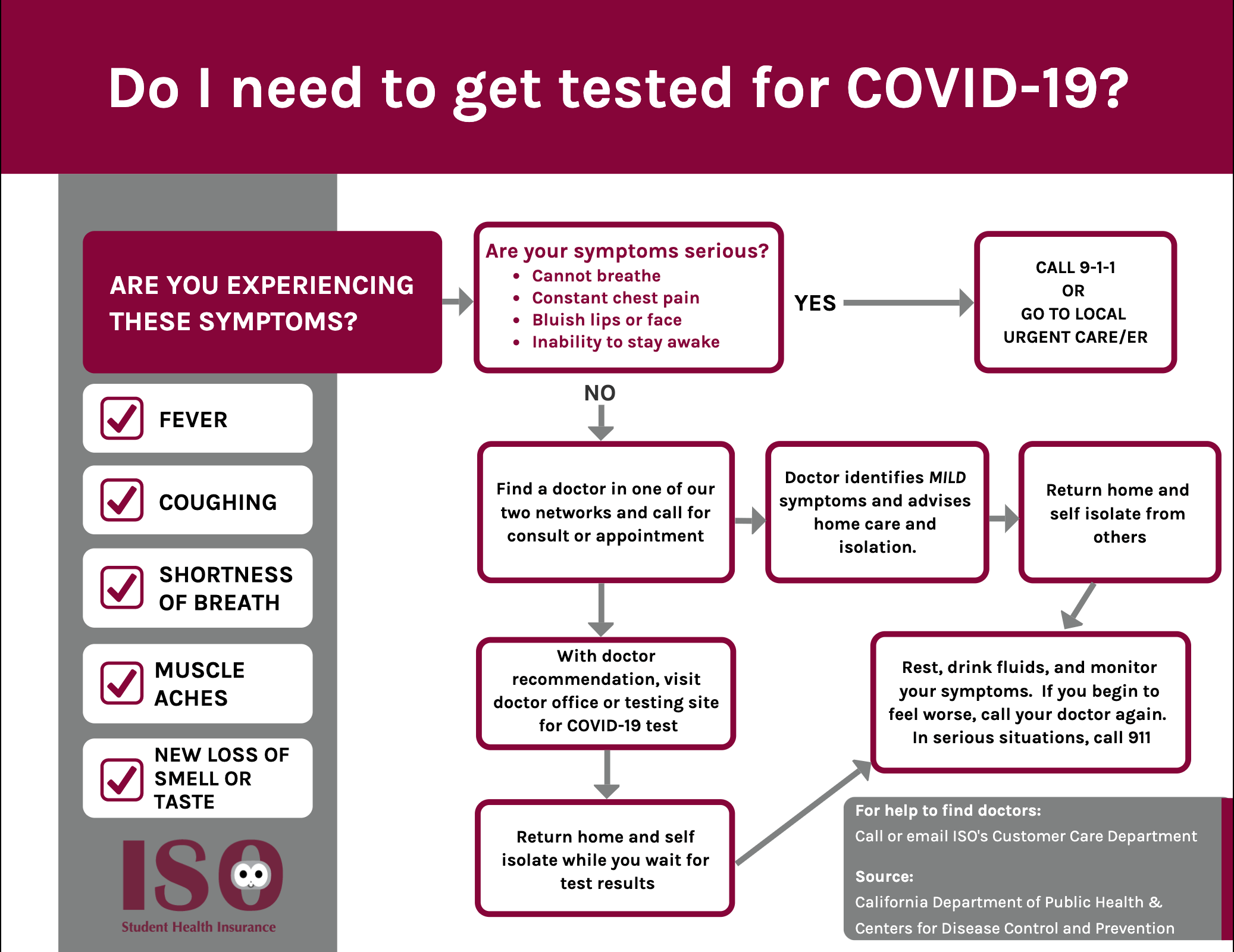
Iso International Student Insurance

Most People Won T Have To Pay For Covid 19 Testing Coronavirus

Centro De Recursos Sobre El Coronavirus Covid 19 Cigna

Centro De Recursos Sobre El Coronavirus Covid 19 Cigna
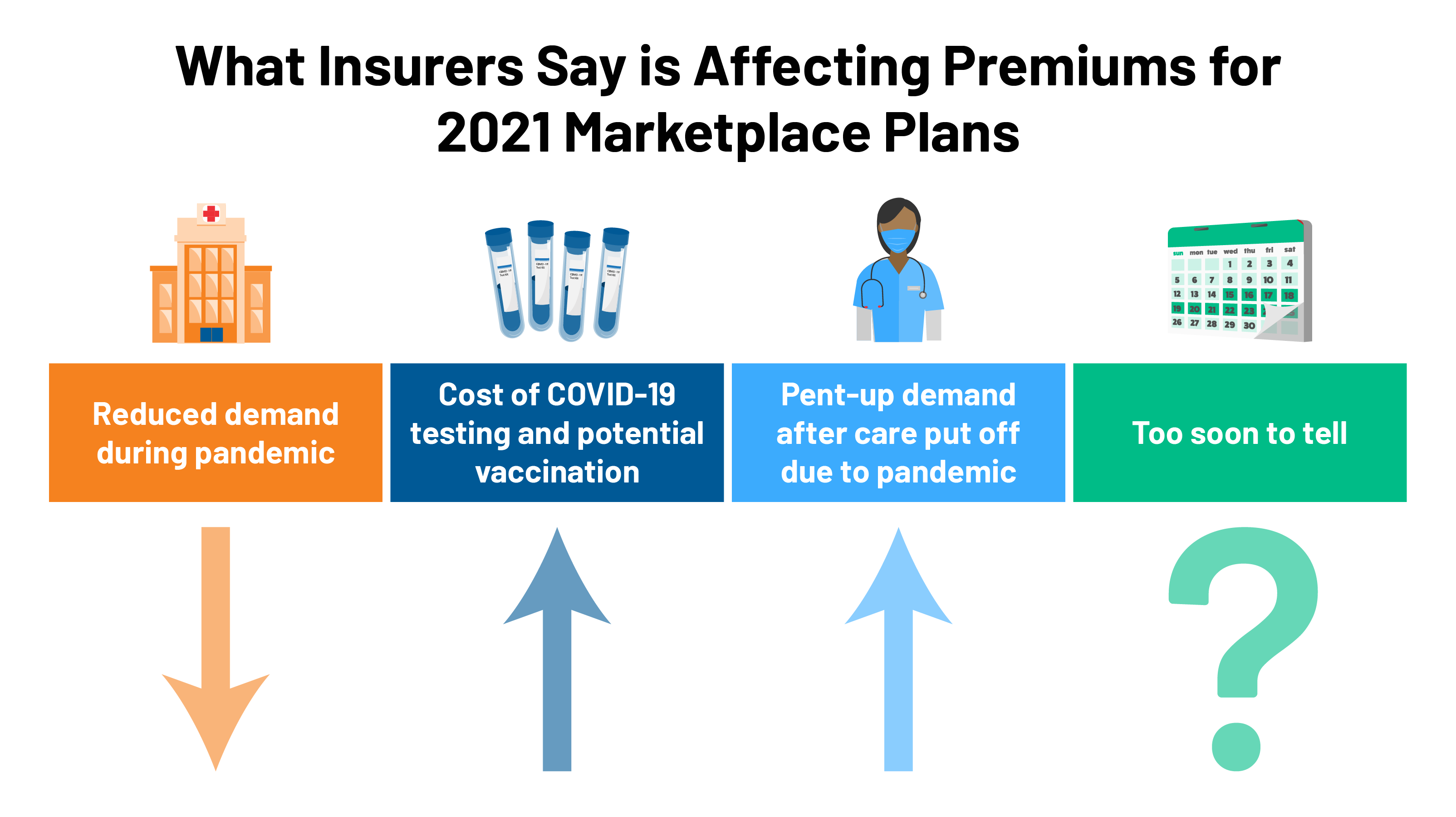
2021 Premium Changes On Aca Exchanges And The Impact Of Covid 19 On Rates Kff

Cigna Covers Cost Of Coronavirus Tests For Customers

Cigna Raises Financial Forecast For 2021 Despite The Ongoing Covid 19 Pandemic Healthcare Finance News

What To Know About Coronavirus Your Insurance Utah Insurance Department

Cigna And Humana Waive Coronavirus Treatment Costs

Dental Benefits Employees Cone Health

Covid 19 Resources For Health Care Access In Washington State Northwest Health Law Advocates
Posting Komentar untuk "Cigna Health Insurance Cover Covid Testing"