Does Health Insurance Cover Rapid Covid Test
These tests are only covered when required by applicable law and adjudicated in accordance with the members benefit plan. The cost of a COVID-19 test should be fully covered by health insurance and a person doesnt have to have symptoms or exposure to someone who tested positive to get one.
.png)
Insurance And Takaful Industry Covid 19 Testing Fund For Medical Insurance Policyholders
Will be covered by Cigna cost share waived.
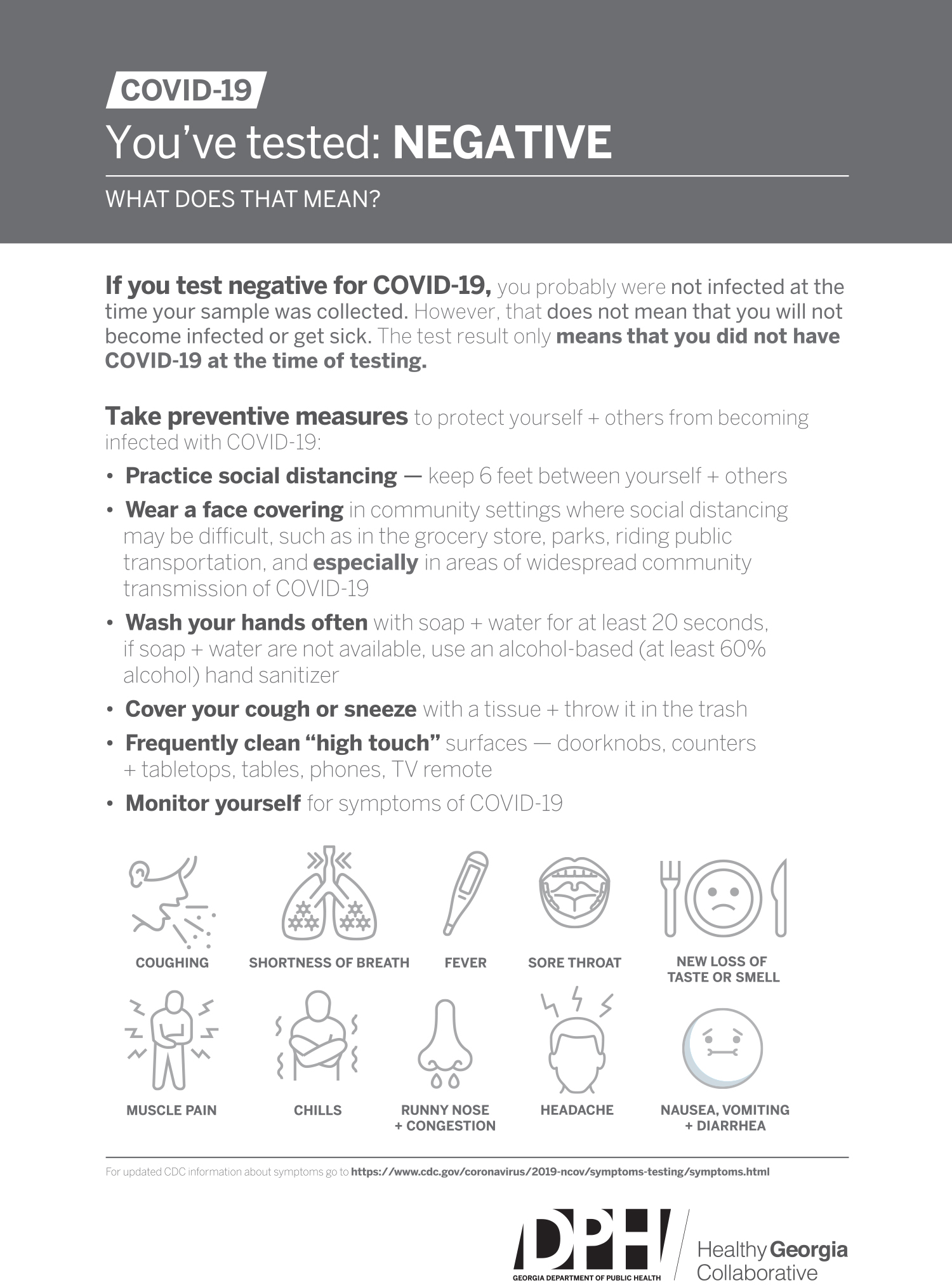
Does health insurance cover rapid covid test. At-home tests obtained without a doctor or providers order are not covered. UnitedHealthcare health plans do not cover COVID-19 surveillance testing which is testing used for public health or social purposes such as employment return to workplace education travel or entertainment. Tests must be provided or ordered by a healthcare provider licensed or authorized to provide or order COVID-19 tests.
Commonly known as COVID-19 PCR test or simply PCR the State Health Plan covers this test at no member cost when prescribed by a healthcare provider for individuals who are symptomatic and for those who have been exposed to COVID-19 and are concerned about infection for the purpose of identifying and treating the disease. Standard PCR tests sent to a lab. Those self-funded employer plans do not have to conform to any.
Coronavirus COVID-19 Health Insurance FAQs. Aetna providers we are here to support you during the coronavirus pandemic with timely answers to the most frequently asked questions about state testing information and other patient care needs. Medicare covers these tests at different locations including some parking lot test sites.
Some that charge travelers for rapid and PCR tests and some that offer complimentary screenings for travelers. When are COVID-19 tests. Americas Health Insurance Plans is calling on more government support to cover the cost of COVID-19 tests which it says could be between 6 billion and 25 billion annually.
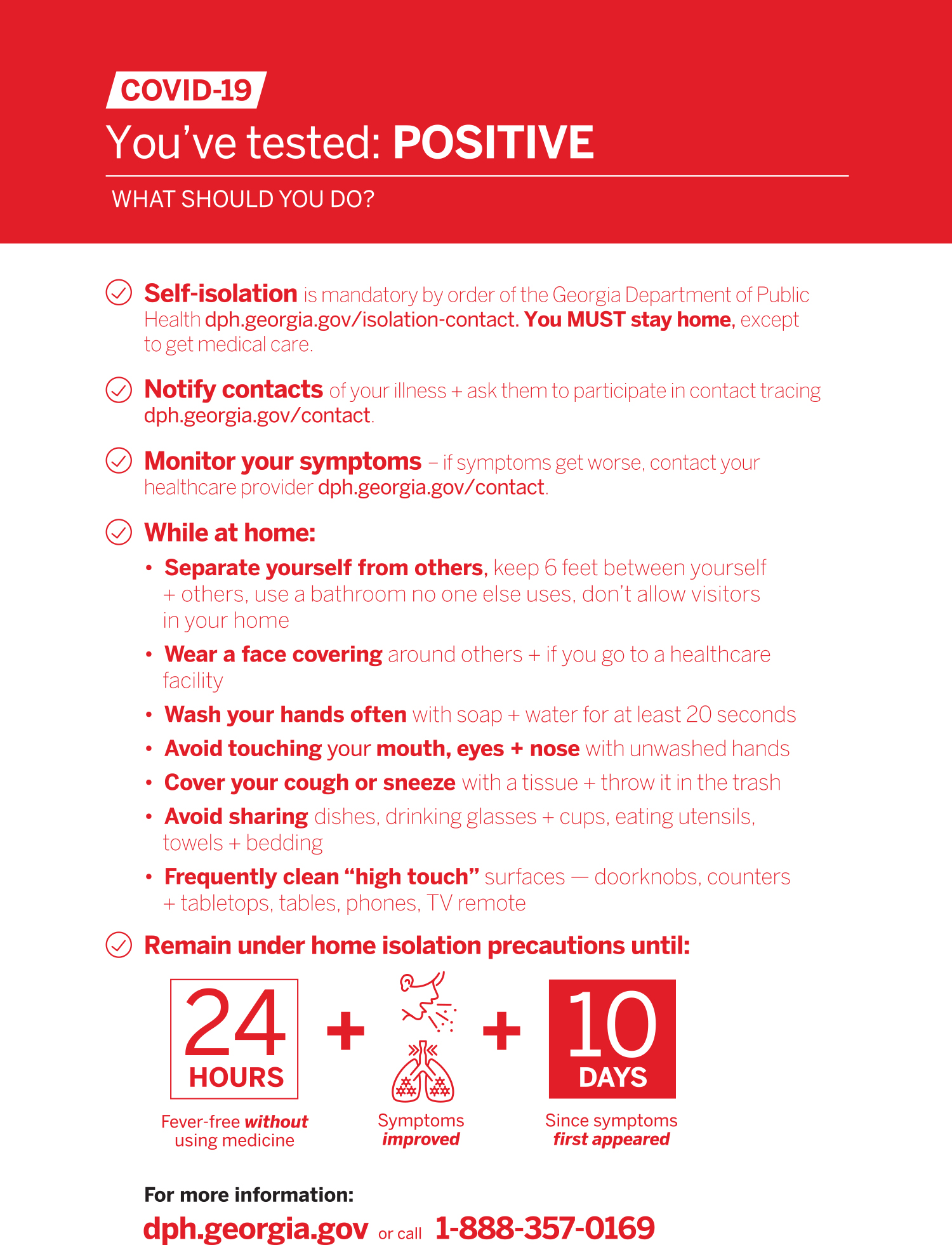
Youll need a negative COVID-19 viral test to re-enter the United States as well. When tests are available for you in your state Medicare covers and you pay nothing for. 2 Rapid-result tests can be pricey costing up to 250 and often arent covered by health insurance.
Individuals can get. Employer sponsored self-funded health plan are regulated by the US Department of Labor under ERISA. These tests are only covered when required by applicable law and adjudicated in accordance with the members benefit plan.
Collect your own specimen by following the detailed instructions. HealthPartners covers COVID-19 diagnostic tests when theyre 1 ordered by a doctor or appropriately licensed provider AND 2 for medically necessary purposes. Based on information gathered from the five largest health insurance companies in the United States there is no limit on how many free COVID-19 tests an insured member can receive.
Complete an online screening. Rapid point of care antigen tests where results are available within a few minutes Home test kits when ordered by a licensed healthcare provider. Tests to diagnose or aid the diagnosis of COVID-19.
Since the legislation was passed on March 18 2020 all forms of public and private insurance are required to cover the costs of COVID-19 testing using tests. UnitedHealthcare health plans do not cover COVID-19 surveillance testing which is testing used for public health or social purposes such as employment return to workplace education travel or entertainment. Learn more about Aetnas coverage policies and guidelines for COVID-19 testing treatment and pricing for patients and providers.
The Connecticut Department of Insurance regulates fully insured health insurance plans issued in the State of Connecticut only. Blue Shield and Blue Shield Promise cover these diagnostic tests. Whether you conduct your COVID-19 test at home or at a clinic if its ordered by a licensed health care professional who believes its medically appropriate then federal legislation requires your private health plan to cover the cost said Sabrina Corlette a research professor who studies health insurance policy at the Center on Health Insurance Reforms at Georgetown.
If your doctor or other health care professional provides a prescription or order for the over-the-counter COVID-19 test as part of clinical care you may submit a claim for reimbursement with both the prescription and detailed receipt to UnitedHealthcare. LabCorp will mail your specimen kit to you. Many airports are now offering test sites.
Provide your Cigna insurance information. Some tests for related respiratory conditions to aid diagnosis of COVID-19 done together with the COVID-19 test.
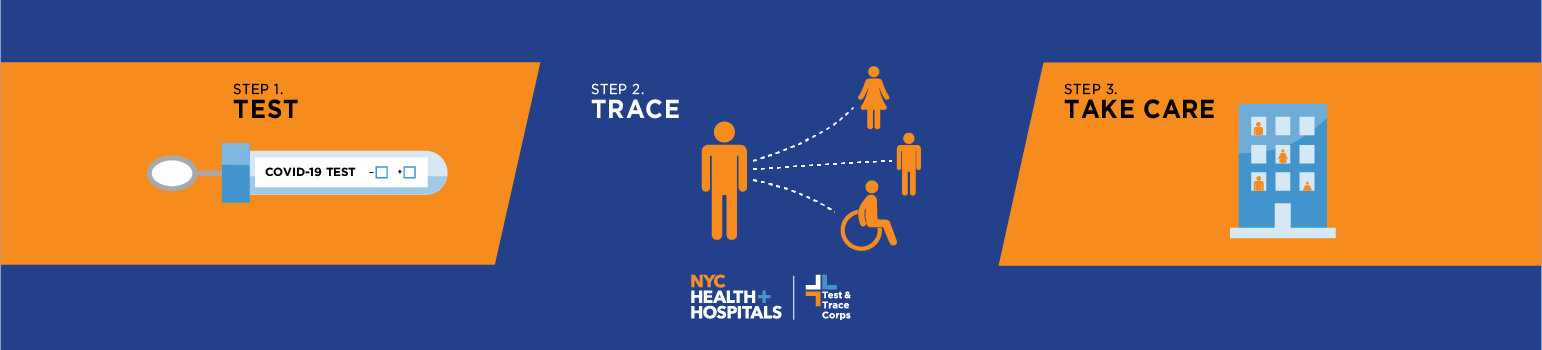
Test Trace Corps Testing Nyc Health Hospitals
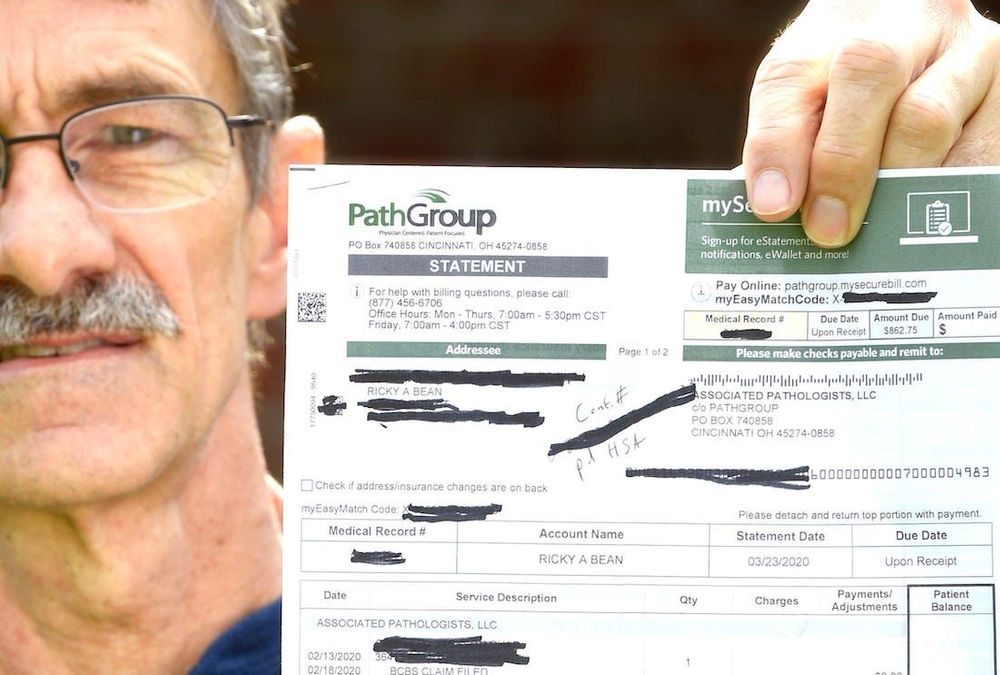
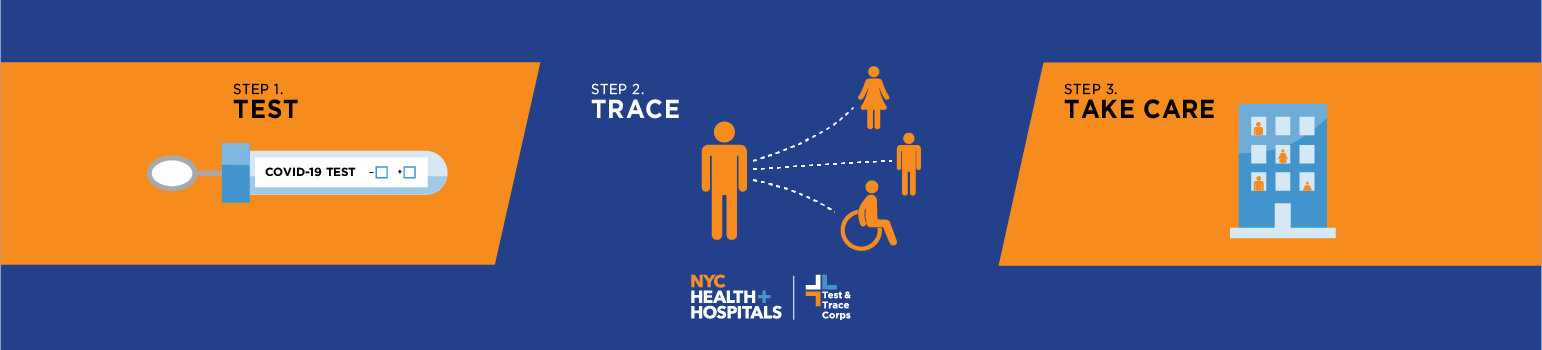
How Much Does A Rapid Covid 19 Test Cost Without Insurance Mira
![]()
Covid 19 Test Prices And Payment Policy Peterson Kff Health System Tracker

Rapid Covid 19 Testing Vitalcare Primary And Family Care

Drive Through Covid Testing Lafayette Concord Pleasant Hill Livermore Click To Register To Schedule

How Americans Can Get A Covid Test In Mexico The Washington Post

Drive Thru Covid 19 Testing Clinic Near Me Covid Clinic

Millions Of At Home Covid Rapid Tests Risk Going Uncounted By Us Bloomberg

Five Things To Know About The Cost Of Covid 19 Testing And Treatment Kff
Antigen Testing For Covid 19 Is Now Available In South Africa Discovery

Rapid Covid 19 Testing Urgent Care Omaha Bellevue Ne Clinics

Covid 19 Testing Anne Arundel County Department Of Health

Antigen And Molecular Tests Types Of Covid 19 Tests

Sars Cov 2 Covid 19 Diagnosis By Igg Igm Rapid Test Clinisciences

Rapid Covid Tests What You Should Know About Accuracy

Covid 19 Testing Urgent Care Of The Palm Beaches

Posting Komentar untuk "Does Health Insurance Cover Rapid Covid Test"