Is Covid Testing Covered By Aetna
Original Medicare covers COVID-19 testing with no out-of-pocket Medicare costs to you. COVID-19 antibody testing is not yet available in MinuteClinic locations in the state of Nevada but is coming soon.
What S In A Covid 19 Test Northwell Health
Learn about extra benefits and well-being resources just for you find testing locations get answers to the most frequently asked questions regarding COVID-19 and tips to stay safe and much more.

Is covid testing covered by aetna. Together were preventing diagnosing and treating diseases with greater precision an approach we call The Keck Effect. This member cost-sharing waiver applies to all Commercial Medicare and Medicaid lines of business. Aetna Better Health of New Jersey is working to protect you from COVID-19 scams.
And its subsidiary companies are not responsible or liable for the content accuracy or privacy practices of linked. Aetna will waive co-pays for all diagnostic testing related to COVID-19 according to CVS Health. About Keck Medicine of USC The Keck Effect Keck Medicine of USC is a world-class academic medical center that attracts the worlds top physicians and researchers.
Aetna Better Health and Aetna Better Health Kids covers testing screening and office visits to diagnose or treat COVID-19. Coronavirus cases in the United States have topped more than 86000 as of Friday morning according to Johns Hopkins data. Up to and including 31 March 2021 Aetna International members will be covered for one test per calendar month if they are asymptomatic and classified as high-risk - as referred by a medical practitioner and when testing takes place in an appropriate medical facility.
You do not need to obtain a referral from a physician in order to get a COVID-19 test and have it covered by Medicare. To ensure access for COVID-19 testing and have consistent reimbursement Aetna will reimburse contracted and non-contracted providers for COVID-19 testing as follows in accordance with the members benefit plan 3. As stated above we only cover COVID-19 diagnostic testing when a member has been referred by a licensed physician.
CHIP members are not to be charged their standard copayments for testing screening or office visits related to COVID-19. UnitedHealthcare health plans do not cover COVID-19 surveillance testing which is testing used for public health or social purposes such as employment return to workplace education travel or entertainment. Do not respond if you get a call text or email about free coronavirus testing.
Recognising the ongoing impact of the pandemic the temporary extension of covid-19 testing coverage will continue. We suggest you check directly with them to learn more about your coverage. Insurance Non-Covered for Rapid COVID Test Medicaid Keystone First Health Partners Aetna Better Health UHC Community Plan Generally Rapid COVID-19 testing is not covered but standard NAA testing is usually covered.
Aetna is going a step further by covering inpatient hospital admissions for COVID-19 treatment and related health complications the insurer said. And second youre in luck. Will members have co -pays for COVID -19 related services.
That includes all member costs associated with diagnostic testing for Commercial Medicare and Medicaid lines of business. The following rates are used for COVID-19 testing for commercial and Medicare plans unless noted otherwise. I f the test is recommend ed by an attending health care provider and the provider writes an order for the test the Families First Coronavirus Response Act requires coverage for the order of and administration of the.
Will mandatory testing be covered. Many insurers youve seen in the news like Blue Cross Blue Shield Aetna and Cigna have announced that if you or someone in your family gets COVID-19 you wont have to. Aetna is here for you during the coronavirus COVID-19 pandemic no matter what.
Aetna is not limiting the number of diagnostic testing we will cover for members however all tests must still meet the requirements listed in this section for coverage. Coronavirus antibody testing must be covered free of charge feds say. Tests for the coronavirus are covered by Medicare Part B much like many other tests and screenings.
These tests are only covered when required by applicable law and adjudicated in accordance with the members benefit plan. Our world-class medical facilities are staffed by over 500 physicians. Under the terms of the Families First Coronavirus Response Act HR6201 Medicare Medicaid and private health insurance plans including grandfathered plans are required to fully cover the cost of COVID-19 testing without any cost-sharing or prior-authorization requirements for the duration of the emergency period which has most recently been extended through mid-April 2021.
You are now being directed to the CVS Health COVID-19 testing site Links to various non-Aetna sites are provided for your convenience only. Aetna Better Health will cover the cost of diagnostic testing related to COVID-19 for Medicaid members. In accordance with guidance from the Centers for Medicare Medicaid Services CMS all health plans must cover certain serological antibody testing with no cost-sharing.
The test can be done by any approved testing facility. The test can be done by any authorized testing facility. Some countries require COVID-19 testing for travelers on arrival.
Most health insurance providers have waived costs related to the testing and treatment of COVID-19. Visit our COVID-19 FAQ page for answers to the most frequently asked questions regarding the coronavirus and to get the latest information. 86408 effective August 10 2020 86409 effective August 10 2020 86413 effective September 8 2020 0224U effective June 25 2020 0226U effective August 10 2020 Coverage of COVID -19 Multiplex Laboratory Testing.
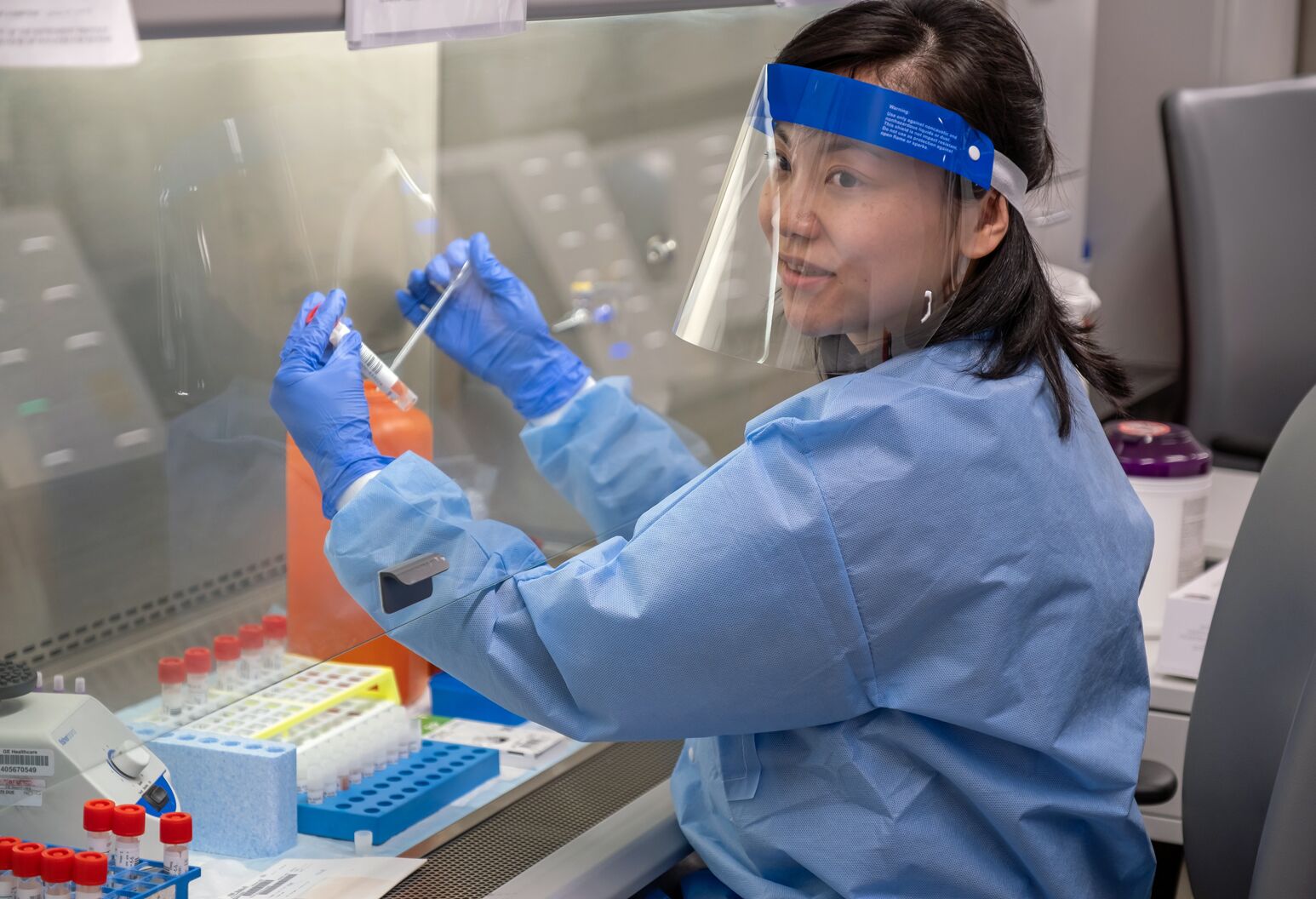
If covered by Medical Assistance or CHIP. Histowiz lab scientists preparing to test COVID-19 samples from recovered patients on April 8 2020. In addition Aetna is waiving member cost-sharing for diagnostic testing related to COVID-19.
Do not give out your Aetna Better Health of New Jersey member ID number or other personal information. COVID-19 antibody testing at MinuteClinic is an extension of CVS Healths overall commitment to providing convenient access to COVID-19 testing and will also be offered in select CVS Pharmacy locations nationwide in the coming weeks. Coverage of COVID -19 Antibody and Viral Neutralizing Laboratory Testing.
If you have Aetna health insurance you can visit their site here to review Testing Treatment FAQs which include details about coverage and authorizations for COVID-19 expenses. Members Aetna is here to keep you informed during the coronavirus COVID-19 pandemic. 87428 effective November 10 2020.
Is COVID-19 related treatment covered.

Does Your Health Insurance Cover You For Covid 19 Cbs News
Coronavirus Covid 19 Allina Health Aetna

Aetna Para Proveedores Del Cuidado De Salud Recursos Y Apoyo Para Profesionales De La Salud

Covid 19 Testing Bills Surprise New Yorkers Crain S New York Business

Aetna Cigna And Humana Waive Most Costs To Patients For Covid 19 Treatment Shots Health News Npr

What To Know About Coronavirus Your Insurance Utah Insurance Department
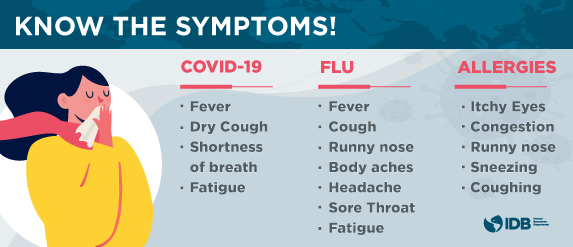
Covid 19 Coronavirus Information Page Iadb

Recursos Relacionados Con El Coronavirus Covid 19 Para Los Miembros De Aetna

Planes De Seguro De Salud Individuales Y Familiares Aetna

A Nurse S View Caring For Covid 19 Patients Northwell Health

Recursos Relacionados Con El Coronavirus Covid 19 Para Los Miembros De Aetna
.jpg)
Recursos Relacionados Con El Coronavirus Covid 19 Para Los Miembros De Aetna

Recursos Relacionados Con El Coronavirus Covid 19 Para Los Miembros De Aetna
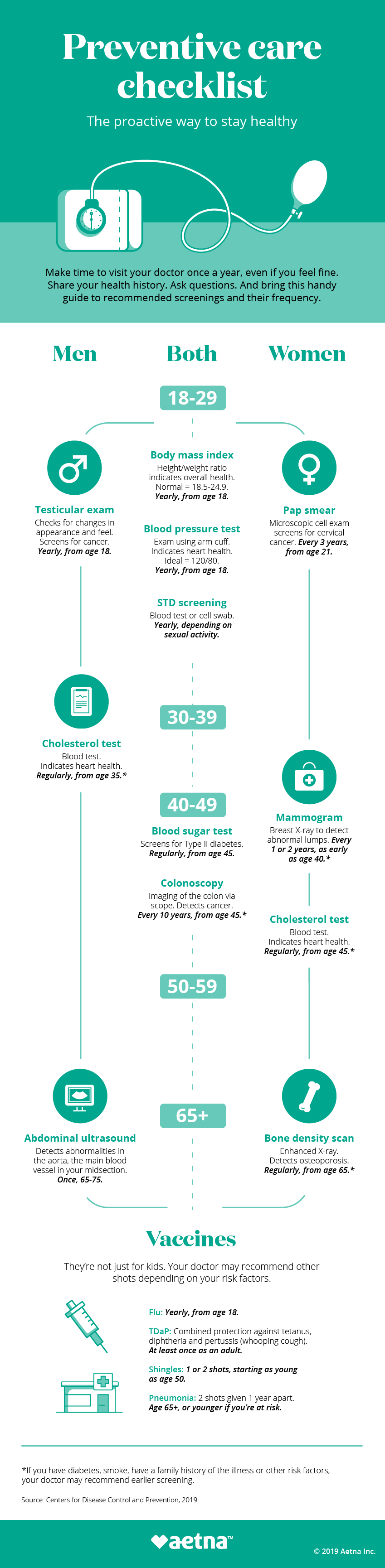
Que Es El Cuidado Preventivo Aetna Pautas De Salud Por Edad

Aetna Better Health Of Louisiana Selected To Participate In Primary Care First Program Cvs Health

Coronavirus Covid 19 Allina Health Aetna

Cvs Pharmacy Locations To Administer Covid 19 Vaccinations When Authorized And Available Cvs Health
Posting Komentar untuk "Is Covid Testing Covered By Aetna"