Does Blue Cross Blue Shield Cover Covid Antibody Test
However we do cover the cost of testing if a health care provider orders an FDA-approved test and determines that the test is medically necessary. You will need an appointment for most of these sites.
Blue Cross Nc To Cover Member Cost Of Coronavirus Test
Tests that are not ordered by a clinician and not related to diagnosis or treatment -- for instance tests required for travel school or work -- may not be covered.

Does blue cross blue shield cover covid antibody test. FEP will waive any cost share for diagnostic tests or treatment that are medically necessary and consistent with CDC guidance if diagnosed with COVID-19. As part of our mission to improve and protect the healthcare system particularly under the threat of the CoronavirusCOVID-19 the Blue Cross Blue Shield Association is focused on protecting members from fraudsters who seek to take advantage of the fear and confusion many feel surrounding the coronavirusCOVID-19 during these uncertain times. All Empire plans cover medically necessary COVID-19 testing and the care visit where the test takes place with no out-of-pocket costs.
This waiver will last through the end of the PHE. Blue Shield will not cover antibody tests unless ordered by a healthcare provider licensed to order COVID-19 tests and for a rare case in which it is needed to help make a diagnosis. As a result providers should not bill BCBSRI for any Medicare Advantage Plan services.
Tests to diagnose COVID-19. At-home tests that have been ordered by an attending healthcare provider and that are approved by the FDA are covered. Lab tests to diagnose COVID-19.
CareFirst and plan sponsors will cover the full cost of in-network deductibles copays and coinsurance for FDA-authorized and medically necessary antibody testing when ordered by a doctor nurse practitioner or other authorized provider. COVID-19 testing at temporary or pop-up testing sites is covered by Blue Shield and Blue Shield Promise without out-of-pocket costs. The vaccine and the administration of COVID-19 vaccines must be submitted to Original Medicare for all patients enrolled in Medicare Advantage in 2020 and 2021.
COVID -19 tests are covered by insurance if they are FDA-authorized and medically necessary. All Anthem plans will cover medically necessary screening and testing for COVID-19 and will waive all cost shares co-pays coinsurance and deductibles. For a vaccine distribution site near.
Medical or invoice records may be requested to support if an antibody test is FDA authorized or if EUA approval has been requested. According to the CDC antibody testing may help support a diagnosis of COVID-19 in people who continue to experience symptoms many days or weeks after the symptoms started. They do not have a lot of openings for unscheduled visits walk or drive-in.
Your Blue Cross and Blue Shield of Texas BCBSTX health plan gives you access to the care you need during the COVID-19 pandemic. Commonly known as COVID-19 PCR test or simply PCR the State Health Plan covers this test at no member cost when prescribed by a healthcare provider for individuals who are symptomatic and for those who have been exposed to COVID-19 and are concerned about infection for the purpose of identifying and treating the disease. Everyone can get tested.
This waiver of cost share is. As announced on April 6 Blue Cross will also waive cost share for COVID 19 related inpatient care at both in- and out-of-network acute care facilities for our fully insured members. With a BCBSTX health plan you have access to care for COVID-19 related health issues.
A doctor must order a COVID-19 test for you. Independent licensees of the Blue Cross and Blue Shield. COVID-19 vaccines reduce the risk of severe disease hospitalization and death and slow spread of the virus.
You may also have to fill out a screening form. Until scientists are able to gather additional data on whether antibodies protect against reinfection of COVID-19 the CDC does not recommend using antibody. Exclusions to this coverage include testing for the following.
This is because COVID-19 antibodies will start to form whether or not the person has recovered. Due to overwhelming interest in our new COVID-19 Vaccination Incentive Program we are extending the deadline for your first dose of a COVID-19 vaccine. July 6 2021.
Your cost share is waived regardless of testing positive or negative for COVID-19. Use the doctors labs and facilities in your BCBSIL health plans provider network for. This includes screenings andor tests that take place at in-person office visits drive-through sites virtual on-line visits and telephone calls.
CODING Medicare Advantage Plans and Commercial Products Monoclonal Antibodies for COVID 19 and. Your Blue Cross and Blue Shield of Illinois BCBSIL health plan gives you access to the care you need during the COVID-19 pandemic. Who can get tested for COVID-19.
Please talk to a doctor first to be certain you need a COVID-19 test. Earn 50 when you get vaccinated by September 6. Independence Blue Cross Independence covers the cost of administering vaccines with no cost-share such as co-pays deductibles coinsurance for members regardless of where the vaccine is given.
For testing performed out of network CareFirst or the plan sponsor will pay 100 up to charge. Does Blue Cross cover the cost of at-home COVID-19 diagnostic tests. Use the doctors labs and facilities in your BCBSTX health plans provider network for.
Now you can earn 50 on your MyBlue Wellness Card when you receive at least one dose by September 6. Blue Cross will cover the cost of FDA-approved COVID-19 diagnostic and antibody tests that are ordered by an attending healthcare provider who determines testing is medically appropriate. With a BCBSIL health plan you have access to care for COVID-19 related health issues.
No Blue Cross doesnt cover the cost of workplace or occupational screening tests for COVID-19. Yes Blue Cross Blue Shield members will not have to pay for COVID-19 diagnostic tests that are performed by a licensed or authorized health care provider through October 18 2021. Blue Cross and Blue Shield of Alabama covers with no member cost share testing that is ordered by your provider to help diagnose or treat you for COVID-19 Is there a vaccine for COVID-19.
BOSTON March 6 2020 PRNewswire -- Blue Cross Blue Shield of Massachusetts Blue Cross has been monitoring and responding to the serious challenges posed by the outbreak of coronavirus strain COVID-19 and we are taking immediate steps to expedite access to testing and care for our members. Member cost-share copay deductibles and coinsurance will be waived for antibody tests that are FDA authorized including tests with Emergency Use Authorized EUA regardless of the diagnosis. Blue Cross members with a COVID-19 diagnosis will be protected against balance billing.

Covid 19 Vaccine Faqs Blue Cross Blue Shield Of Vermont
Benefits Trs Covid 19 Resources
Azblue Coronavirus For Providers

D C Clinic Offers Antibody Coronavirus Test With Results In Minutes For A Price Npr

Your Guide To No Cost Testing And Treatment As Covid 19 Surges

We Re Continuing To Waive Covid 19 Testing And Treatment Costs For Our Members

Covid 19 Antibody Testing Starts For 5 000 Arizona First Responders
Should You Get Covid Antibody Testing And What Do The Results Mean Uab Experts Respond The Reporter Uab

Your Frequently Asked Questions About Covid 19 Coronavirus
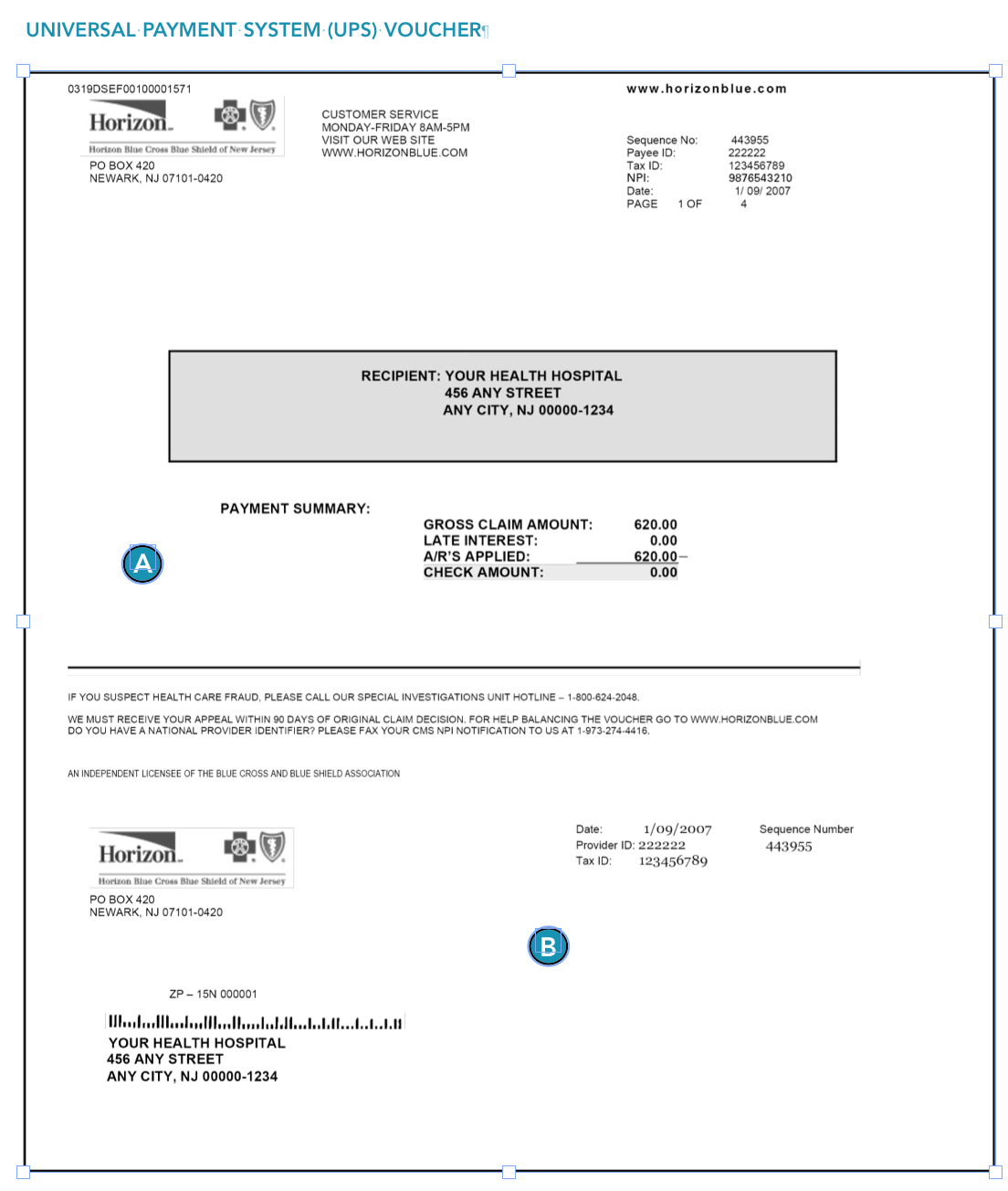
Claims Submissions And Reimbursement Horizon Blue Cross Blue Shield Of New Jersey

Should You Get Covid Antibody Testing And What Do The Results Mean Uab Experts Respond The Reporter Uab
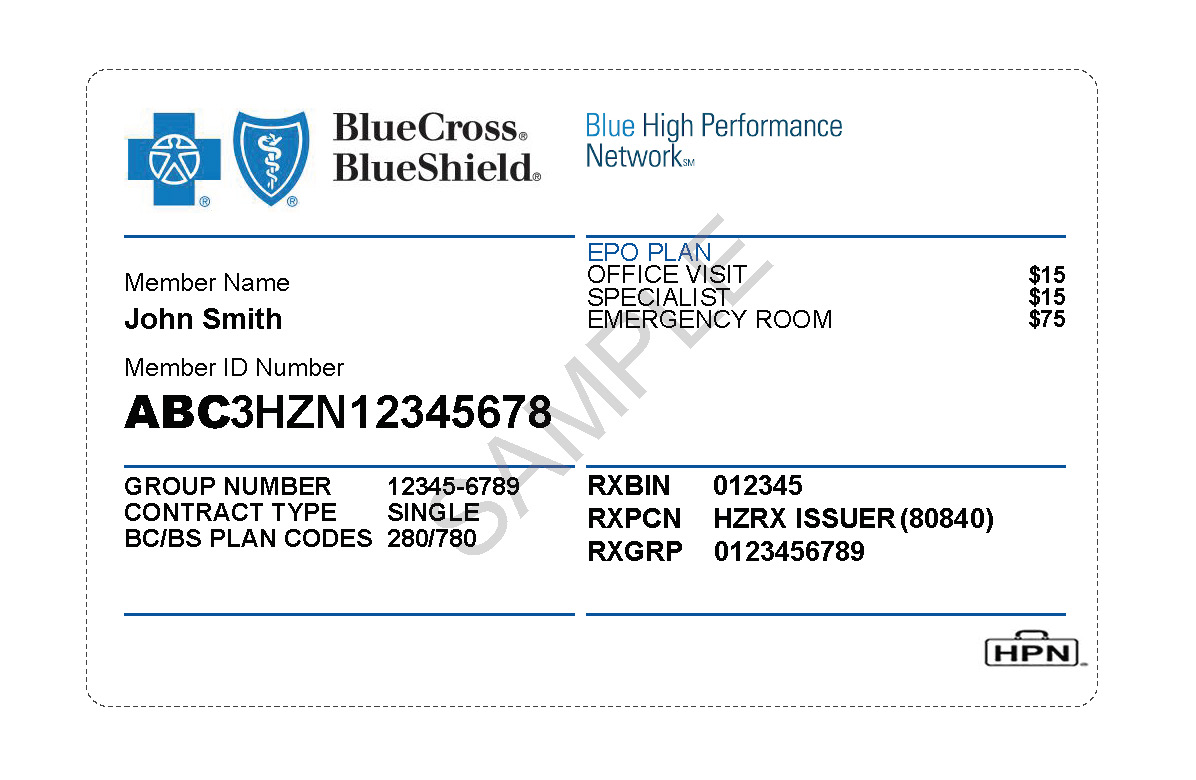
Introducing The Blue High Performance Network Hpn Program Horizon Blue Cross Blue Shield Of New Jersey

Coronavirus Antibody Testing Am Pm Walk In Urgent Care Clinic

Coverage And Costs Highmark Answers

Teamsterscare Bcbs Covid Testing Coverage Teamsterscare 25

Untangling Covid 19 Testing What You Need To Know Regence
What S In A Covid 19 Test Northwell Health

Posting Komentar untuk "Does Blue Cross Blue Shield Cover Covid Antibody Test"