Will Insurance Cover Out Of Network Covid Testing
Cigna covers the cost of administering FDA-authorized COVID-19 vaccines at 100 without any out-of-pocket costs when performed by an in-network or out-of-network provider. Access testing if you need it Cigna is waiving out-of-pocket costs for FDA-approved COVID-19 diagnostic PCR and antigen testing tests.
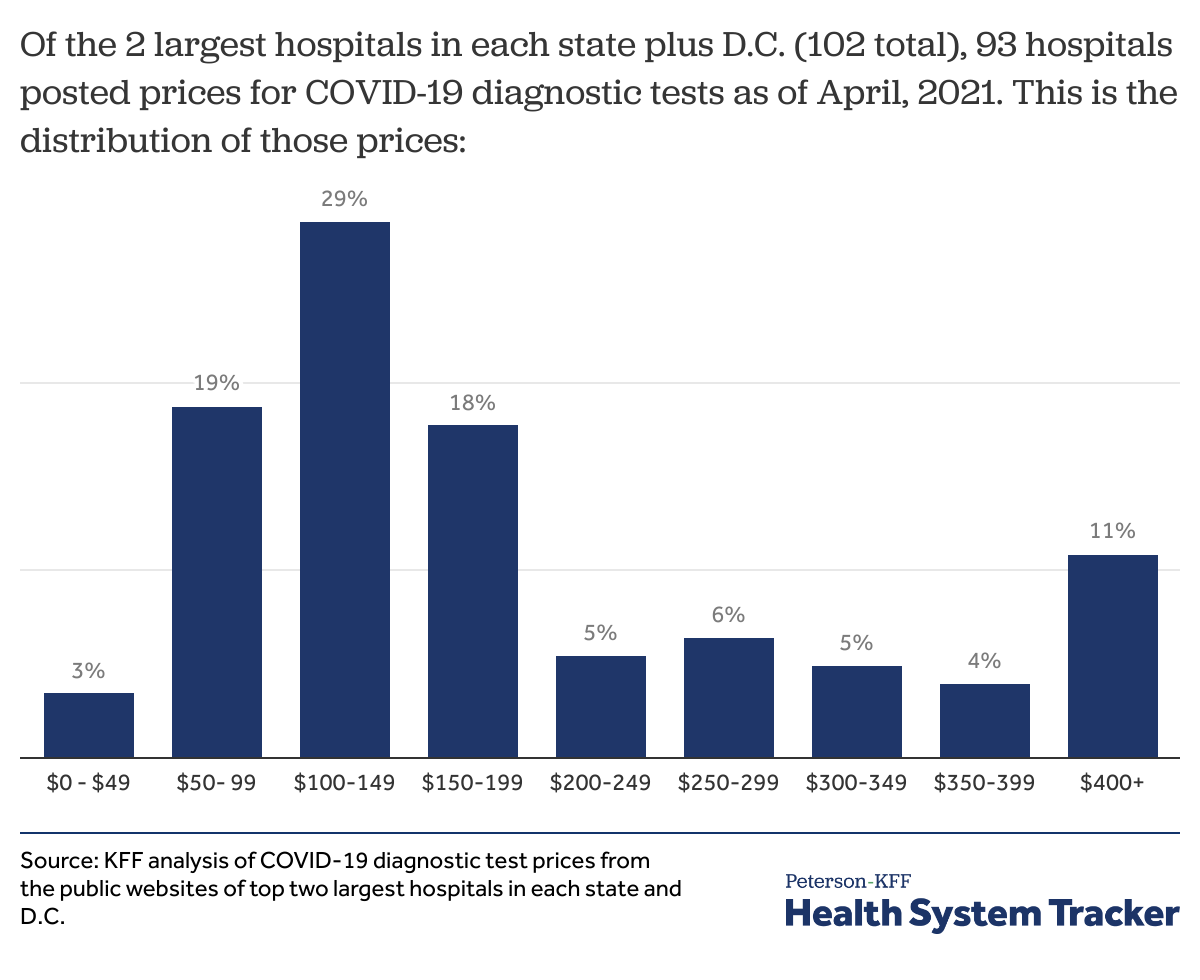
Covid 19 Test Prices And Payment Policy Peterson Kff Health System Tracker
The CARES Act also passed in March 2020 requires that private insurance plans cover out-of-network coronavirus tests and says that if people are charged upfront for testing the patient should.

Will insurance cover out of network covid testing. If there is an issue with accessing care through an in-network provider that would prolong testing for COVID-19 testing performed by an out-of-network provider must be covered by your health insurer at no out-of-pocket cost. Blue Shield and Blue Shield Promise cover most diagnostic tests for individuals at no out-of-pocket cost to you. You have options Cigna is waiving out-of-pocket costs for COVID-19 visits whether.
UnitedHealthcare will reimburse out-of-network providers for COVID-19 testing-related visits and COVID-19 related treatment or services according to the rates outlined in the Medicaid Fee Schedule. Can I see an out-of-network provider for COVID-19 testing if my in-network provider cannot see me. Method the plan generally uses to determine payments for out-of-network services or the amount that would be paid under Medicare.
When are COVID-19 tests covered. Ohio Department of Health Director Amy Acton MD MPH strongly recommends that Ohioans are aware of the following information provided by the Ohio Department of Insurance regarding out-of-network insurance coverage specific to COVID-19 testing and treatment. Connect with a provider.
Under the CARES Act plans and insurers must reimburse out-of-network providers for COVID-19 tests based on the providers publicly listed cash price for the test. UnitedHealthcare will cover medically appropriate COVID-19 testing during the national public health emergency period currently scheduled to end Oct. See below for those not covered This means you do not need to pay out-of-pocket costs copay coinsurance or deductible for tests that are provided or ordered by a healthcare provider.
Then came questions July 28 2021 Under federal law all public and private insurance plans must fully cover any coronavirus test. 17 2021 at no cost share when ordered or reviewed by a physician or appropriately licensed health care professional to either 1 diagnose if the virus. In Washington DC plans are required to cover all out-of-network charges related to COVID-19 testing screening and treatment including cost-sharing and balance billing unless a patient was first offered the.
Effective March 20 2020 the Ohio Department of Insurance issued a bulletin defining. Vaccine guidelines and requirements can vary by state and county. A Pasadena startup got billions selling COVID tests.
Private insurers should be required to pay for out-of-network diagnostic covid-19 testing and associated services at prevailing in-network rates or. Find vaccine information and resources in your state COVID-19 Vaccines Care and Coverage. If you have insurance and sought COVID-19 treatment from an out-of-network provider that has received General or Targeted Distributions from the Provider Relief Fund the provider has agreed not to seek to collect out-of-pocket payments greater than what you would have otherwise been required to pay if the care had been provided by an in-network provider.
If you have individual or group health insurance coverage that you or your employer bought in New York including through the NY State of Health Marketplace or the New York State Health Insurance Program NYSHIP for public employees you are covered for the testing and treatment for novel coronavirus COVID-19 as described below. In-network and out-of-network tests.
![]()
Potential Costs Of Covid 19 Treatment For People With Employer Coverage Peterson Kff Health System Tracker
What Went Wrong With Coronavirus Testing In The U S The New Yorker

Carson Coronavirus Testing By Us Health Fairs
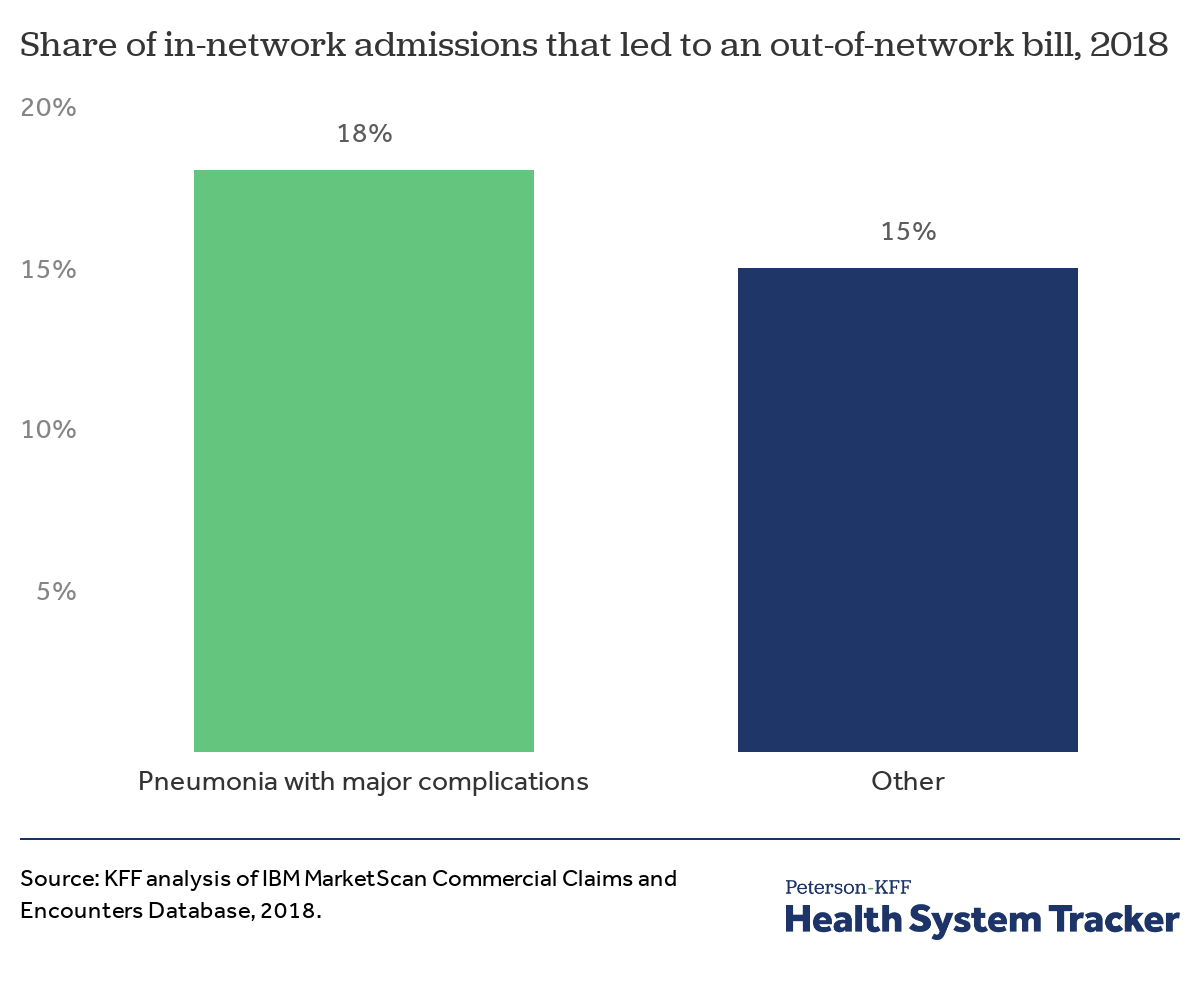
Potential Costs Of Covid 19 Treatment For People With Employer Coverage Peterson Kff Health System Tracker

Coronavirus Covid 19 Tests Methods Availability And Accuracy

Testing Information For Covid 19 Mount Sinai New York

Covid 19 Testing Sites Nyc Health Hospitals
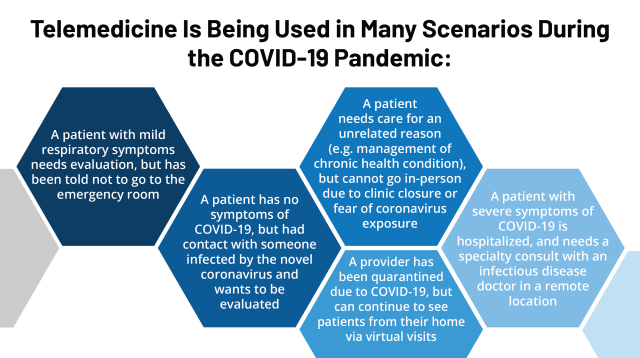
Opportunities And Barriers For Telemedicine In The U S During The Covid 19 Emergency And Beyond Kff

Carson Coronavirus Testing By Us Health Fairs
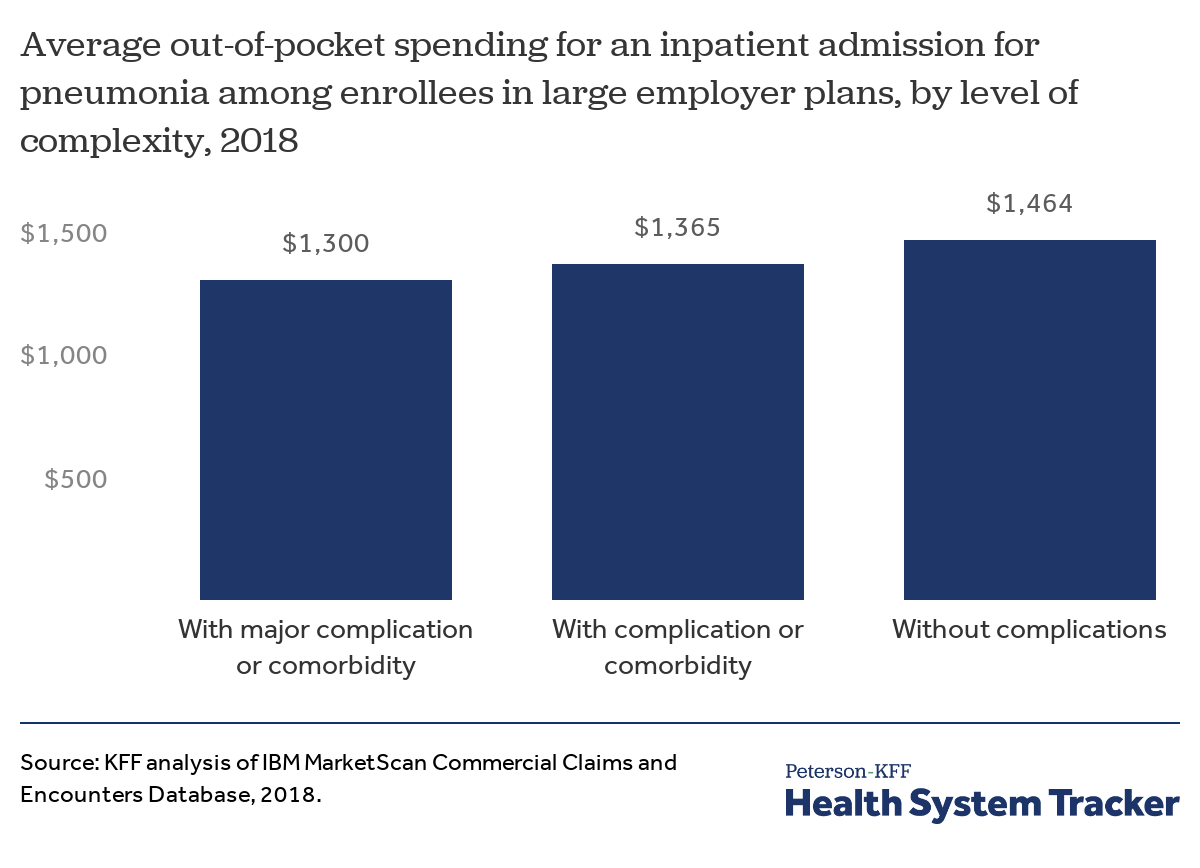
Potential Costs Of Covid 19 Treatment For People With Employer Coverage Peterson Kff Health System Tracker
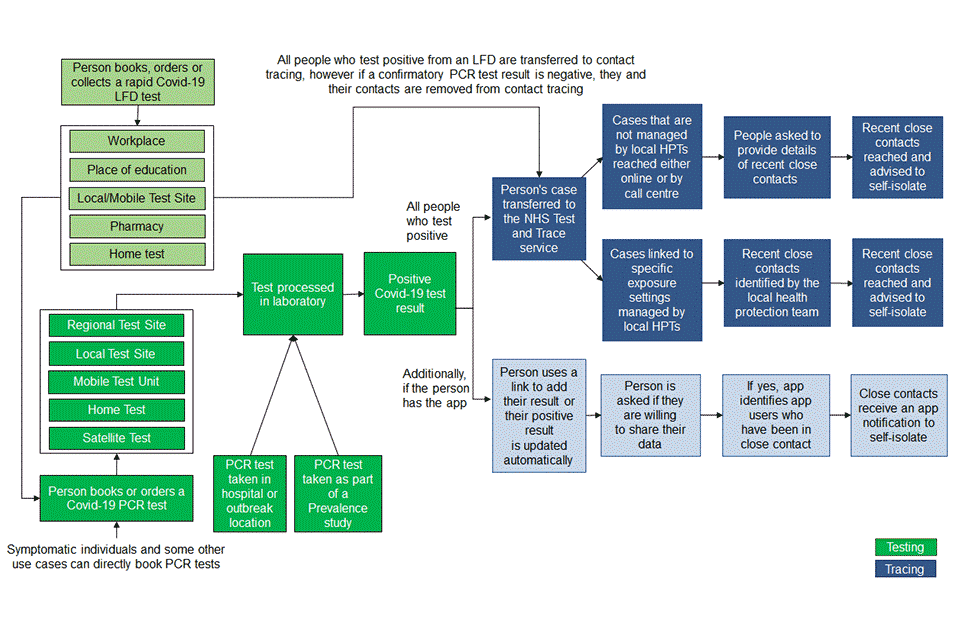
Nhs Test And Trace Statistics England Methodology Gov Uk

Drive Through Covid Testing Lafayette Concord Pleasant Hill Livermore Click To Register To Schedule
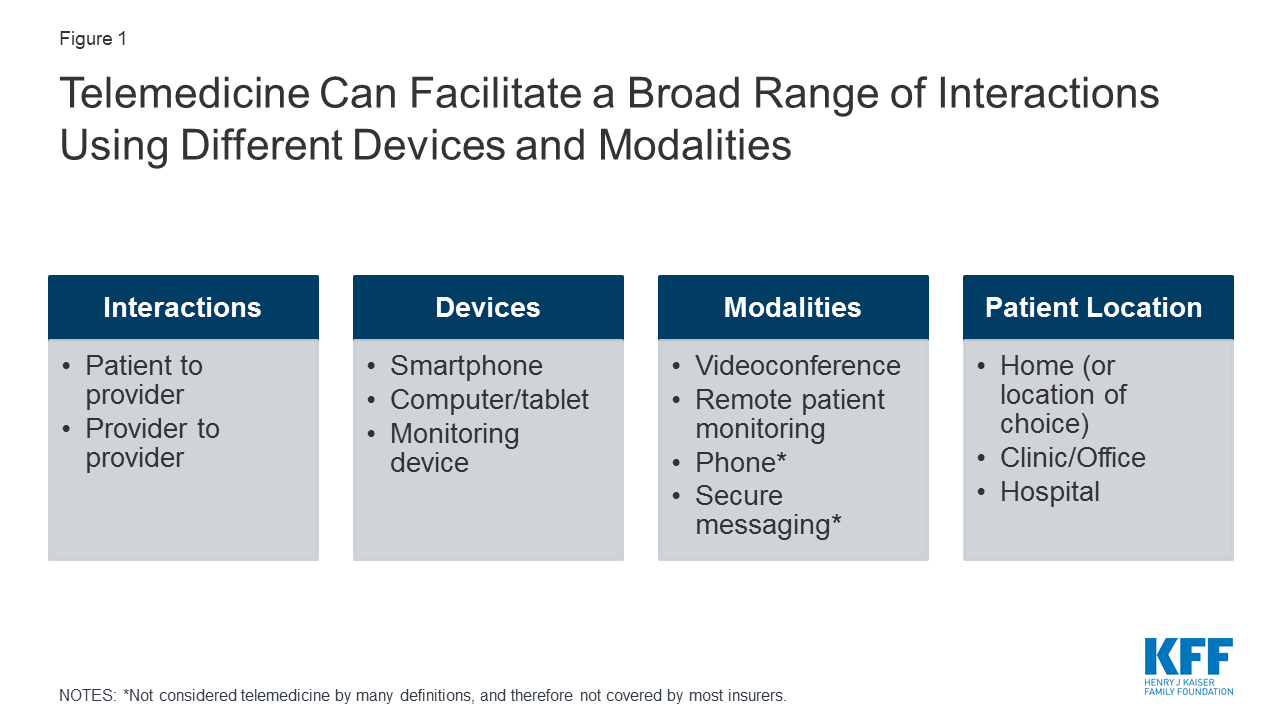
Opportunities And Barriers For Telemedicine In The U S During The Covid 19 Emergency And Beyond Kff

Five Things To Know About The Cost Of Covid 19 Testing And Treatment Kff

A Covid Test Costs 54 000 An Er Told This Patient Shots Health News Npr

Testing For Covid 19 Faqs Blue Shield Of Ca

Coverage For Covid 19 Testing Vaccinations And Treatment Center On Budget And Policy Priorities

Covid 19 Testing Near Me Map Shows Every Site In The San Francisco Bay Area Abc7 San Francisco
Private Health Coverage Of Covid 19 Key Facts And Issues Kff
Posting Komentar untuk "Will Insurance Cover Out Of Network Covid Testing"