Are Covid Tests Covered By Insurance United Healthcare
TrustAssures healthcare provider network ensures that customers are given options for COVID-19 RT-PCR tests that satisfy entry requirements for the US including the required testing timeframe. Original Medicare covers COVID-19 testing with no out-of-pocket Medicare costs to you.
Private Health Coverage Of Covid 19 Key Facts And Issues Kff
COVID-19 testing would continue to be covered with no cost-sharing by private and public insurers for all tests consumers independently seek but the federal government would pay directly for.
/cdn.vox-cdn.com/uploads/chorus_asset/file/19808102/GettyImages_1212276863.jpg)
Are covid tests covered by insurance united healthcare. Many airports are now offering test sites. And second youre in luck. If your doctor or other health care professional provides a prescription or order for the over-the-counter COVID-19 test as part of clinical care you may submit a claim for reimbursement with both the prescription and detailed receipt to UnitedHealthcare.
Is the test for COVID-19 antibodies covered by my insurance. UnitedHealthcare will cover medically appropriate COVID-19 testing at no cost share during the national public health emergency period currently scheduled to end Oct. Federal law requires all private insurance plans to cover the entire cost associated with approved COVID-19 testing so long as the test is deemed medically appropriate.
UnitedHealthcare health plans do not cover COVID-19 surveillance testing which is testing used for public health or social purposes such as employment return to workplace education travel or entertainment. Medicare Advantage clients with a positive diagnosis can receive monoclonal antibody treatment at no cost through 2021. Can arrange an appointment for a local COVID-19 test through United and TrustAssure.
Doctors typically charge about 50 to 100 for the tests so the costs of weekly testing could add up quickly. Some have reinstated them. Is Covid hospital treatment covered by insurance.
If you do not have health insurance talk to any health care provider in your area to see if they will agree to bill the federal government for other COVID-19. These tests are only covered when required by applicable law and adjudicated in accordance with the members benefit plan. Youll need a negative COVID-19 viral test to re-enter the United States as well.
But plans that arent considered minimum essential coverage arent required to cover COVID-19 testing. Prior authorization is not needed for diagnostic tests and covered services that are medically-necessary and follow COVID-19 CDC guidelines. State variations and regulations may apply.
Congress required health plans to fully cover COVID-19 testing but insurance companies are starting to argue they should only have to pay if patients show symptoms or tests are ordered by a. Based on information gathered from the five largest health insurance companies in the United States there is no limit on how many free COVID-19 tests an insured member can receive. COVID-19 vaccines are 100 free for every individual living in the United States - even if you do not have insurance.
Tests for the coronavirus are covered by Medicare Part B much like many other tests and screenings. You may be able to set up a telehealth visit to talk to a provider from your home both for routine medical care and for care related to COVID-19. Private health insurance plans to cover COVID-19 testing administration of the test and related items and services without consumer cost sharing.
Find COVID-19 coverage information and learn how to access resources and support. And over at Allianz Global Assistance which offers COVID-19 insurance and assistance for clients who test positive for COVID-19 while travelling a COVID-19 test will only be a covered cost under. Some that charge travelers for rapid and PCR tests and some that offer complimentary screenings for travelers.
You do not need to obtain a referral from a physician in order to get a COVID-19 test and have it covered by Medicare. Standard cost-sharing applies for COVID-19 treatment with one exception. The Coronavirus Aid Relief and Economic.
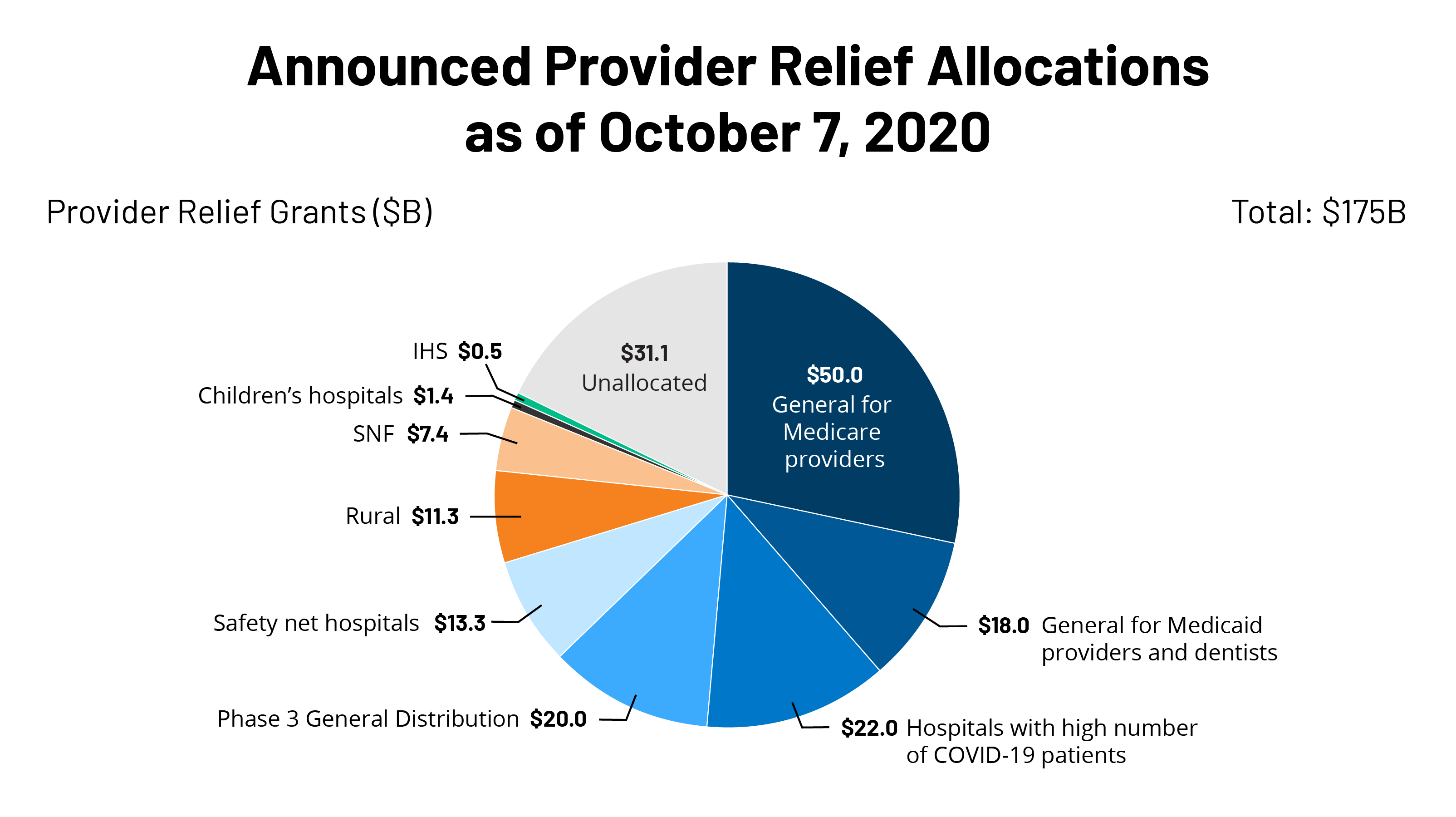
Travelers originating from outside the US. Department of Health and Human Services HHS provides claims reimbursement to health care providers generally at Medicare rates for testing uninsured individuals for COVID-19 treating uninsured individuals with a COVID-19 diagnosis and administering COVID-19 vaccines to uninsured individuals. Government pre-paid for COVID-19 vaccines and required COVID-19 vaccines be made available at no out-of-pocket costs regardless of whether the vaccine recipient is insured.
Federal law requires insurers to fully cover the tests when ordered by a health. AlohaCare will fully cover medically-necessary diagnostic tests for COVID-19 according to the Centers for Disease Control and Prevention CDC guidelines. Insurers voluntarily set aside charges earlier in the pandemic.
Yes a federal law called the CARES Act provides that tests for COVID-19 antibodies are covered without a copayment coinsurance or deductible when your attending healthcare provider determines that the testing is medically appropriate for you. 2 Rapid-result tests can be pricey costing up to 250 and often arent covered by health insurance. Even though the COVID vaccine is free retail pharmacies like CVS and Publix are asking for insurance information when booking appointments and asking patients to.
However while a handful. Insurers not required to pay for mandatory employer COVID-19 tests HHS says New guidance also covers telehealth coverage and balance-billing for testing-related services. A separate program the HRSA COVID-19.
COVID-19 tests purchased OTC without a prescription or health care professionals involvement such as those bought at a pharmacy or online and processed without a lab or health care professional involvement are not covered by the members benefits plan Members will be responsible for the cost of OTC tests. UnitedHealthcare is here to serve during this unprecedented time. 17 2021 when ordered by a physician or appropriately licensed health care professional for purposes of the diagnosis or treatment of an individual member.
Under the Families First Coronavirus Response Act Medicare Medicaid and private health insurance plans are required to fully cover the cost of COVID-19 testing. No out-of-pocket costs for FDA-approved diagnostic tests ordered by a health care professional or for testing-related visits during the federal public health emergency.

If You Get A Coronavirus Test Will Insurance Pay It Depends Shots Health News Npr

Covid 19 Testing Hennepin Healthcare
![]()
Covid 19 Test Prices And Payment Policy Peterson Kff Health System Tracker

Five Things To Know About The Cost Of Covid 19 Testing And Treatment Kff
/cdn.vox-cdn.com/uploads/chorus_image/image/66505723/GettyImages_1212276863.0.jpg)
The Covid 19 Coronavirus Exposed Weaknesses In The Us Health System Vox
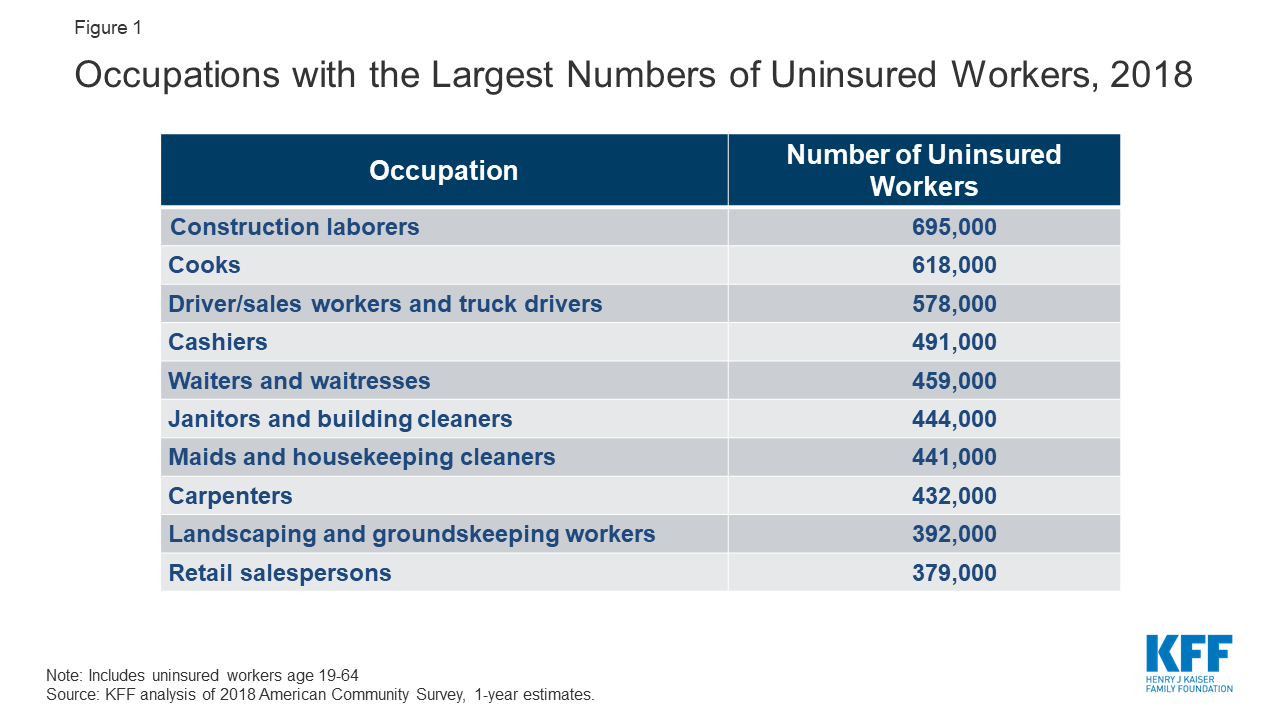
What Issues Will Uninsured People Face With Testing And Treatment For Covid 19 Kff
/cdn.vox-cdn.com/uploads/chorus_asset/file/19786951/covid_19_testing_per_capita.jpg)
The Covid 19 Coronavirus Exposed Weaknesses In The Us Health System Vox

Coronavirus Covid 19 Tests Methods Availability And Accuracy
![]()
Travel Care The Right Insurance Cover For Your Trip Lufthansa

How Home Coronavirus Testing Could Slow Disease Spread

How Americans Can Get A Covid Test In Mexico The Washington Post
Limitations Of The Program For Uninsured Covid 19 Patients Raise Concerns Kff
/cdn.vox-cdn.com/uploads/chorus_asset/file/19808102/GettyImages_1212276863.jpg)
The Covid 19 Coronavirus Exposed Weaknesses In The Us Health System Vox

In The Coronavirus Pandemic We Re Making Decisions Without Reliable Data
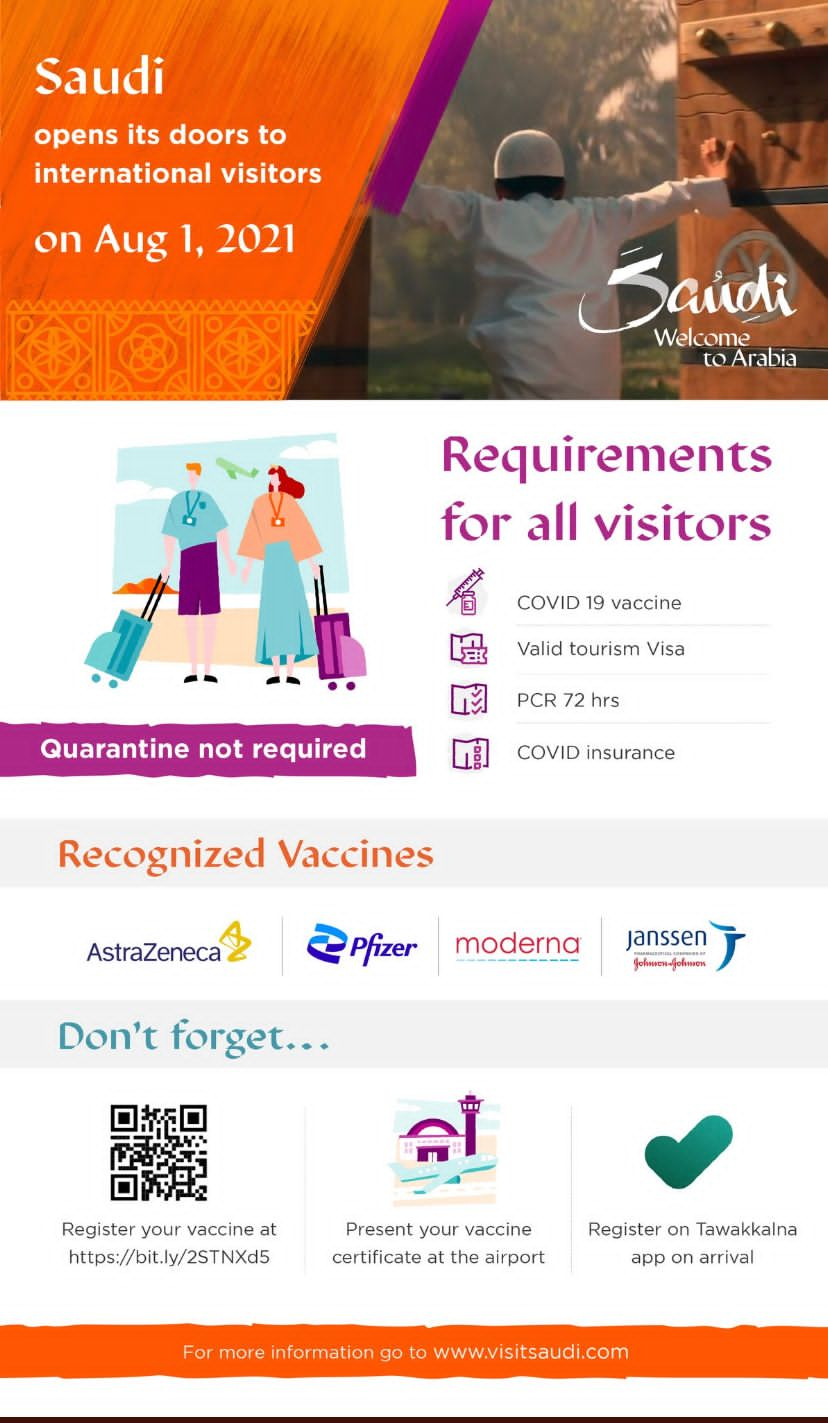
Traveling To The Kingdom After Covid 19 Pandemic The Embassy Of The Kingdom Of Saudi Arabia

Student Essay The Disproportional Impact Of Covid 19 On African Americans Health And Human Rights Journal
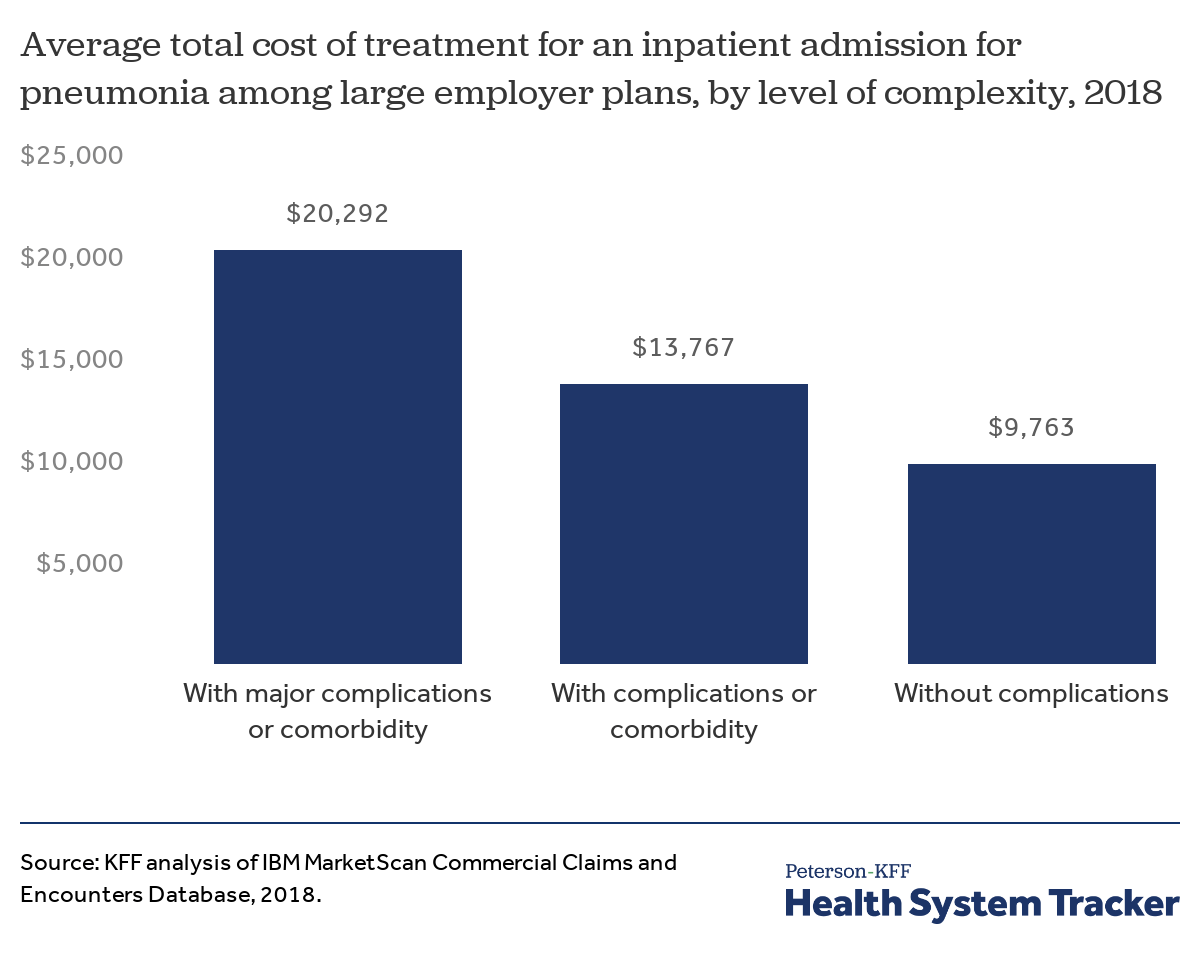
Potential Costs Of Covid 19 Treatment For People With Employer Coverage Peterson Kff Health System Tracker
![]()
Potential Costs Of Covid 19 Treatment For People With Employer Coverage Peterson Kff Health System Tracker

Posting Komentar untuk "Are Covid Tests Covered By Insurance United Healthcare"